Written by Pendell Meyers with edits by Smith
A man in his early 40s with history of HTN presented to the ED for feeling lightheadedness and mild "beating" chest pain off and on last night, but resolved at the time of ED presentation. He still felt some lightheadedness during evaluation. He stated that he used ecstasy yesterday prior to the onset of symptoms. Vitals were within normal limits on arrival.
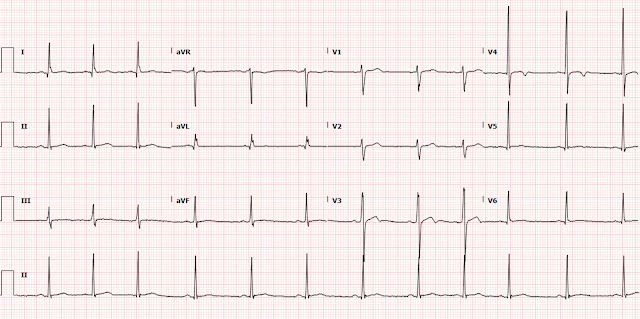 |
| What do you think? |
A 40-something healthy male with transient chest squeezing
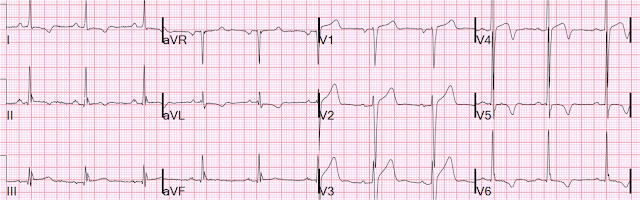
Classic Evolution of Wellens' T-waves over 26 hours
Back to the case:
The patient had a prior ECG on file from 6 months ago:
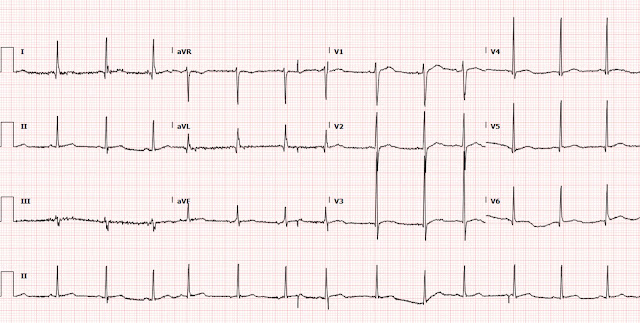 |
| No TWI here. Tiny amount of normal variant STE in lateral leads. |
It is certainly appropriate to measure troponins, and so 3 serial high sensitivity troponin I measurements were all ⋖ 6 ng/L (below the limit of detection, normal 99% URL for men for this assay is 20 ng/L).
Repeat ECG 4 hours after arrival:
 |
| The T wave may be a tiny bit deeper in V3, but overall there is not much change. Side by side is below. |
Despite no further chest pain, no evolution of ECG findings, and three serial negative troponins, the ED team was concerned for Wellens.
3 serial negative troponins should suffice in a case like this to rule out ACS.
However, the providers advised the patient that he should be admitted for further risk stratification. The patient declined and signed out against medical advice.
Learning Points:
There are many causes and patterns of T-wave inversion. And among them, many can mimic Wellens pattern (which is simply anterior reperfusion T wave inversion). There are some clinical features that help distinguish them, and expert ECG interpretation can help a great deal to distinguish them. Bottom line: see a bunch of them, follow up the results, and compare them to the cases we've posted - you will become great at it.
Normal variant patterns can change over time.
True reperfusion T wave inversions must evolve over time (must either progress through the reperfusion sequence of deepening T wave inversions, or resolve due to very brief reversible ischemia, or reocclude!). If any T wave inversion pattern does not evolve at all over serial ECGs, then it is not due to ischemia.
If a patient has reperfusion T waves that are evolving along the reperfusion sequence (becoming full T wave inversion and deeper), then there has been substantial ischemia even though there is some reperfusion, and Dr. Smith and I believe it is almost guaranteed that there will be a rise and fall detected in appropriately timed serial high sensitivity troponins.
It is possible that this rise and fall in Wellens' might be below the URL; for example:
Result: < 6 ng/L → 12 ng/L → 17 ng/L → 9 ng/L → < 6 ng/L
See these other cases involving Wellens mimics:







No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.