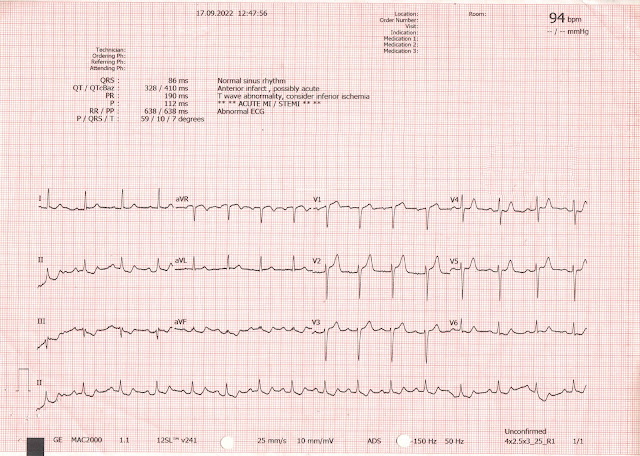
I was texted this ECG:
The ECG is diagnostic of acute inferior-posterior OMI. This is what I texted back:
"It is tricky because it is in the setting of left ventricular hypertrophy. And I worry the cardiologist will say that it is all LVH. But I am quite certain that it is diagnostic of acute OMI. And if you find an old one, it will not look like this."
"See V2: there is downsloping ST segment . The T wave in lead III Is too big for that small S wave. There is terminal QRS distortion in aVF. The STT in aVF is not discordant as you would expect with LVH, and there is a straight ST segment."
I sent it to Pendell, and he immediately texted back:
"Nice inferior-posterior OMI. Likely to be missed."
The MD who sent it to me is a highly skilled, fellowship trained ED ultrasonographer. She did a bedside echo and did not see any wall motion abnormality.
Later, I heard the history:
A 40-something male with past medical history significant only for hypertension presented to the ED with acute onset of chest pain, associated with diaphoretic and shortness of breath.
At the time of the 2nd ECG, his chest pain is improving however still present. No similar episodes of chest pain in the past.
He had presented through triage (not by ambulance) 1.25 hours after pain onset, and the ECG was recorded another 27 minutes later (our ED is completely overwhelmed with patients who are "boarding" in the ED and in triage is thus also overwhelmed on a daily basis)
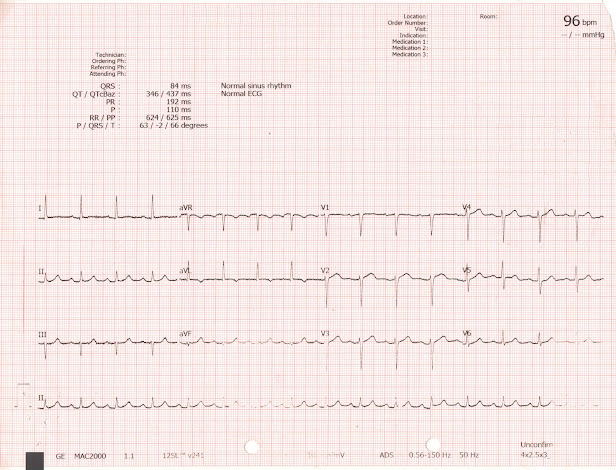
The cath lab was activated, and a 2nd ECG was recorded 55 minutes after the first one, while waiting for the cath team:
Angiogram:
RCA: dominant. It supplies a medium sized RPDA (right posterior descending) and small RPLA (right posterolateral). It is thrombotically or embolically occluded in the distal segment at the bifurcation to the RPDA and RPLA. It was successfully stented.
Formal Echo with Definity Bubble Contrast:
Decreased left ventricular systolic performance, mild; estimated left ventricular ejection fraction is 45%.
Regional wall motion abnormality- mid to distal inferior segments ("posterior" is no longer recognized as an echocardiogram wall, but this amounts to an inferior and posterior MI)
Highest hs troponin I measured (at 6 hours, after PCI -- which releases "pent up" troponin) = 24, 500 ng/L.
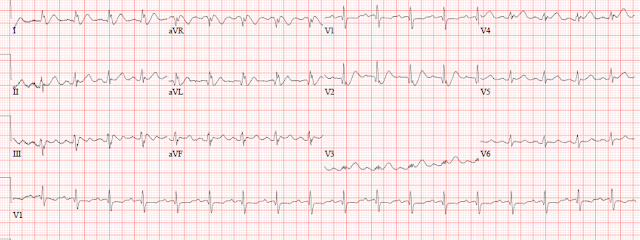
An ECG was recorded the next day:
Echocardiography, even (or especially) with Speckle Tracking, can get you in trouble. The ECG told the story.
What happens when a patient with LAD OMI does not go immediately to the cath lab?
===================================
MY Comment, by KEN GRAUER, MD (9/30/2022):
===================================
- I focus my comment on a few additional aspects to those discussed above by Dr. Smith that I hope will be useful for approaching this diagnostic dilemma.
- For clarity in Figure-1 — I've reproduced the initial ECG that was texted to Dr. Smith without the benefit of any history. For comparison — I have added the chest leads from a patient with LVH but no acute OMI (taken from the July 29, 2022 post in Dr. Smith's ECG Blog).
-USE.png) |
| Figure-1: The initial ECG that was texted to Dr. Smith ( = ECG #1). Compare the chest leads of ECG #1 — with the chest leads in ECG #2 (which I've taken from the 1st case presented in Dr. McLaren's July 29, 2022 post in Dr. Smith's ECG Blog). |
- Per Dr. Smith: "There is a downsloping ST segment in lead V2".
- Per Dr. Smith: "The T wave in lead III is too big for that small S wave. There is terminal QRS distortion in lead aVF — and the ST segment in this lead is straight".
- The abnormal shape of the ST-T wave in lead V2 constitutes a positive Mirror Test. Even without LVH — the taller-than-expected initial R wave in lead V2 and the ST-T wave appearance in this lead instantly suggested to me that posterior OMI was likely (Please see My Comment at the bottom of the page in our recent September 21, 2022 post — in which I review in detail my use of the Mirror Test).
- In a normal tracing (ie, without LVH) — the ST segment in leads V2 and V3 is very often slightly elevated, with a gentle upsloping — that leads into a positive T wave. So in addition to the definitely abnormal shape of the ST-T wave in lead V2 — I immediately thought lead V3 in ECG #1 was highly suspicious of a continuation of an acute process.
- Knowing that leads V2 and V3 were abnormal quickly convinced me that the disproportionately large (hypervoluminous) ST-T wave in lead III almost certainly represented a hyperacute T wave. And as soon as I found out that the patient in question presented with new-onset chest pain — the diagnosis of acute infero-postero OMI was assured until proven otherwise.
- PEARL: In my experience, the fragmented QrS complex in lead III is virtually diagnostic of infarction at some point in time. Much more than a simple negative deflection (ie, Q wave) — the finding of an initial negative deflection (Q wave) — that then briefly turns positive (the small r that we see in lead III) — but which then promptly descends again (into the deep S wave) — is indicative of scar, and most often of infarction at some point in time. Given the hyperacute ST-T wave in lead III — this strongly suggests an ongoing acute process!
- The presence of increased voltage on ECG without ST-T wave abnormality consistent with LV "strain" (or a "strain equivalent" pattern) — is not specific for true LV chamber enlargement. In such cases (IF there is a need to know) — Echo would be needed to distinguish between benign increased QRS amplitude on ECG vs true chamber enlargement.
- In contrast — in a patient with the "right disease" (ie, heart failure, longstanding hypertension) — who is of a certain age (ie, younger adults often manifest increased QRS amplitude not due to chamber enlargement) — the finding of voltage criteria for LVH + ST-T wave changes of "strain" is more than 90% specific for true LV enlargement!
- Not all patients with Echo-proven LVH manifest LV "strain" on ECG. The Framingham Studies taught us that longterm prognosis is adversely affected when both voltage and repolarization changes of "strain" are present on ECG.
- ST-T wave changes of LV "strain" are most commonly seen in one or more of the lateral leads (ie, in leads I, aVL; and/or V4, V5, V6). Typically — there is slow descent of the ST segment, with a more rapid rise at the end of the ST segment.
- Some patients with LVH (especially if the frontal plane axis is vertical) — also manifest ST-T changes of LV "strain" in the inferior leads.
- Some patients with especially deep anterior S waves — manifest the "mirror-image" picture of LV "strain" in the form of an upright ST-T wave, often with some ST elevation in these anterior leads.
- The other major effect produced by LVH on ECG is that the increase in leftward and posterior forces forces may overshadow baseline anterior forces — with a "net result" that R wave progression is delayed (sometimes to the point of producing QS complexes in one or more anterior leads).
- Voltage criteria for LVH are fulfilled in multiple leads in ECG #1. These include: i) One or more limb leads with an R wave ≥20 mm; ii) R in aVL ≥12 mm; iii) Deepest S in V1,V2 + tallest R in V5,V6 ≥35; and, iv) R in V6 ≥18 mm.
- A classic LV "strain" pattern is seen in lead aVL (and to a lesser extent in lead I). To Emphasize — the slowly downsloping ST segment shape with more rapid return to baseline in lead aVL is so typical, that even with possible added effect from reciprocal OMI changes — I interpreted this ST-T wave appearance in these high-lateral leads as typical for LV "strain".
- The patient in today's case is 40-year old man who has hypertension — therefore, he is clearly in a higher prevalence group likely to have true LVH.
- KEY Point: Despite multiple leads showing markedly increased voltage — the chest leads in ECG #1 are remarkable because: i) There is no ST-T wave elevation in any of the anterior leads; and, ii) Although there is shallow T wave inversion in leads V5 and V6 — there is virtually no slowly downsloping ST segment depression in these leads (as would be expected in a patient such as this with so much other ECG evidence for true LVH with "strain").
- BOTTOM LINE re ECG #1: Given the history of new-onset severe chest pain — the logical conclusion is that the lack of the typical LV "strain" changes in anterior and lateral chest leads is because the acute infero-postero OMI produced opposing ST-T wave changes that attenuated what we otherwise would have seen from LV "strain".
- As mentioned above — the 6 chest leads in ECG #2 are from a patient with marked LVH but no acute OMI.
- As sometimes happens — Instead of manifesting increased lateral chest lead R wave amplitude — this patient manifests exceedingly deep anterior S waves in leads V1 and especially V2 (I've outlined in RED the huge >30 mm S wave in lead V2).
- Considering how deep the S wave in lead V2 is — the ST elevation with large, peaked T wave in this lead is not disproportionate — and was purely the result of marked LVH.
- Although lateral chest leads V5 and V6 show no more than modest R wave amplitude — these leads nevertheless manifest an ST-T wave shape highly typical for LV "strain".
- In CONCLUSION: Contrast a final time the appearance of ST-T waves consistent with LV "strain" in the anterior and lateral chest leads of ECG #2 — with the lack of such changes in the chest leads of ECG #1 (in which ST-T wave changes were attenuated by the opposing effect of the ongoing acute infero-postero OMI).










-USE-copy.png)



-USE.png)
