This 70-something woman with no significant past history (no previous ECGs or cardiac history) presented by EMS with fairly acute chest pressure and shortness of breath, with nausea and diaphoresis. "Like an elephant sitting on my chest." She had no history of atrial fibrillation and was not on any anticoagulants.
She stated that she had had a similar episode a couple weeks earlier, lasting 24 hours, with rapid heart beat but without chest pain, that spontaneously resolved. She thought she was having a panic attack. Since then she has had "little spurts" of the same thing lasting 1-2 hours.
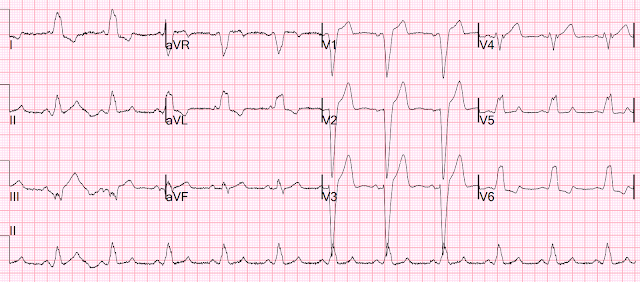
EMS EKG was recorded:
Smith: This is a wide complex tachycardia. But it is an IRREGULAR wide complex tachycardia, so it is indeed atrial fibrillation with rapid ventricular response. But it is impossible to say much about "STEMI" or "Occlusion MI" or "Ischemia" because the QRST goes off the page in both directions. Moreover, whenever there is Atrial fibrillation with a rapid ventricular response, ESPECIALLY when there is LBBB, the ECG can mimic Occlusion when no Occlusion is present.
EMS activated the cath lab prehospital. When she arrived, an ED ECG was recorded:
Bedside Echo of low technical quality showed a few B lines, no volume depletion, and moderately decreased contractility.
Because of the risk of stroke from thromboembolism, they did not perform cardioversion. She was given 5 mg IV metoprolol, which slowed the rate a bit. She was given enoxaparin as well.
Another ECG was recorded 1.5 hours after the first:
The first hs troponin I was 23 ng/L. It peaked at 47 ng/L (URL for women is 16 ng/L). These levels are not consistent with acute coronary occlusion, even if reperfused.
By the next morning, she had spontaneously converted to sinus rhythm:
Formal echo day 2, about the same time as the above ECG
Estimated LV ejection fraction-lower limits of normal = 50%. Asynchronous interventricular septal motion-LBBB.
The patient was taken for an angiogram that morning 16 hours after arrival:
No significant disease
Comments:
1. Patients with Atrial Fibrillation with RVR have distorted ST Segments
2. Tachycardia in LBBB exaggerates ST Elevation
3. Atrial Fibrillation with RVR can cause acute chest pain and dyspnea, just like acute coronary occlusion (OMI)
4. First, get the heart rate down and then re-assess.
5. There is controversy over when to use cardioversion (electrical or chemical). ACC/AHA guidelines are pasted below. It is important to know that most paroxysmal atrial fib will spontaneously convert within 48 hours (about 70%). One might argue that cardioverting earlier allows less time for a thrombus to form.
In any case, there is no good answer to this question:
1. "How unstable does a patient have to be for me to take the risk of stroke and electrically cardiovert atrial fibrillation when the patient is not anticoagulated and we do not know for certain when it started?
Certainly, this depends not only on the risk of remaining in atrial fibrillation, but also the probability that the atrial fib is of remote, vs. recent, onset.
It is also true that, if the atrial fibrillation is long standing, cardioversion is unlikely to be effective.
Nor is there a good answer to these questions:
2. "How CERTAIN do I have to be of the time of onset of atrial fibrillation?" In this patient, it seems pretty clear that the onset was shortly before arrival, but it is not certain. Moreover, atrial fib can be intermittent and thrombus form chronically even if the patient had recently been in sinus rhythm. (But if it is intermittent, then the patient is likely to spontaneously convert and be at the same risk).
3. What is the best AV nodal blocker to use?
--Some say amiodarone, but amiodarone has a high chance (~33%) of converting to sinus, and you are using an AV nodal blocker because you want to AVOID cardioversion (the risk of stroke with chemical and electrical cardioversion is presumably the same).
--Some say esmolol because you can turn it off if there are complications. However, the effect on myocardial contractility of esmolol may not be apparent for hour and the patient may make a slow downhill descent that is not immediately recognized.
--Some say diltiazem, but it also has profound effects on contractility.
Digoxin is ideal, EXCEPT that it takes hours to work; if you have the time, that is fine, but if the patient is truly unstable, then it won't suffice.
Metoprolol worked in this case, but isn't that as bad as esmolol (selective beta-1 blockade)? Our electrophysiologist states that esmolol has more hypotensive effects than other beta-1 selective blockers. I don't know of any literature on that.
Electricity is by far the most likely to work: it not only slows the rate, but may restore the atrial contribution to ventricular filling, if the atrium has not been stunned by prolonged fibrillation. (If it has been stunned, then the danger of cardioversion is mitigated!). Cardioversion does put the patient at higher risk of stroke, but how much higher? I don't think anyone knows. There has not been a randomized trial of electrical cardioversion vs. AV nodal blockade for patients with unstable AF RVR (as far as I know).
What is the answer? I do not know. If the patient has serious ischemia, pulmonary edema, or shock, I electrically cardiovert because the risk of death outweighs the risk of stroke.
This is a fine discussion of the topic at EMdocs.net: http://www.emdocs.net/unstable-atrial-fibrillation-a-guide-to-management/
2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary
https://www.jacc.org/doi/pdf/10.1016/j.jacc.2014.03.021
"Cardioversion
is recommended when a rapid ventricular response to AF or atrial
flutter does not respond promptly to pharmacological therapies and
contributes to ongoing myocardial ischemia, hypotension, or HF. For
patients with AF or atrial flutter of more than 48 hours’ duration or
unknown duration that requires immediate cardioversion for hemodynamic
instability, anticoagulation should be initiated as soon as possible and
continued for at least 4 weeks after cardioversion unless
contraindicated. (Level of Evidence: C)"




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.