Written by Pendell Meyers, case submitted by Tom Fiero
A man in his 30s walked into the ED complaining of chest pain. His triage ECG was done at 11:30 (no prior was available):
Sinus tachycardia
Normal QRS complex pattern, with borderline low voltage
Very slight STE in leads V2-V5
Proportionally large and fat T-waves in V4-5 with straightening of the ST segments
T-waves also concerning in II, III, aVF, with inappropriately negative T-waves in aVL
Using the LAD OMI vs. BER formula:
3 Variable: 27.34 (positive for OMI, using STE60V3=1.5mm, QTc=444, RWV4=2.0mm)
4 Variable: 23.01 (positive for OMI, using QRS amplitude V2=7.5mm) (> 18.2 is most accurate cutoff; > 19.0 is 97% specific)
This ECG was sent to Pendell, Smith, and Grauer. All immediately diagnosed LAD occlusion.
This ECG pattern as a whole is extremely specific for full thickness, complete ischemia of the anterior, lateral, and inferior/apical walls. There are several etiologies of this (including takotsubo cardiomyopathy, coronary spasm, etc), however the overwhelmingly most likely, most important, and most treatable etiology is acute Occlusion MI (OMI), in this case likely a wraparound LAD that supplies the anterior wall and wraps around to the apex (showing up in the inferior leads). The only way to differentiate OMI from other, less treatable causes is emergent angiogram.
This ECG was interpreted as "no STEMI" and the clinician initiated a typical workup for undifferentiated chest pain.
Approximately an hour or two later, the initial troponin I returned positive at 0.8 ng/mL.
A second ECG was ordered after this troponin resulted:
A third ECG was recorded before transport:
The patient was given ASA, heparin bolus, and thrombolytics. He was transferred to the regional PCI center, and the exact cath outcome was very difficult to obtain, however the findings included triple vessel disease with complicated LAD and LCX lesions that required urgent CABG and balloon pump for cardiogenic shock. The ultimate outcome is not obtainable.
Learning Points:
Never exclude OMI based on age. Young people can have OMI.
You should learn to recognize this pattern of wraparound LAD occlusion, including the subtle but diagnostic hyperacute T-waves in V4 from the original ECG.
This young patient likely would have had a much better outcome if his need for emergent reperfusion had been recognized 1-2 hours earlier.
See these other cases of young people with OMI:
See these other similar cases:
A man in his 30s walked into the ED complaining of chest pain. His triage ECG was done at 11:30 (no prior was available):
 |
| What do you think? |
Sinus tachycardia
Normal QRS complex pattern, with borderline low voltage
Very slight STE in leads V2-V5
Proportionally large and fat T-waves in V4-5 with straightening of the ST segments
T-waves also concerning in II, III, aVF, with inappropriately negative T-waves in aVL
Using the LAD OMI vs. BER formula:
3 Variable: 27.34 (positive for OMI, using STE60V3=1.5mm, QTc=444, RWV4=2.0mm)
4 Variable: 23.01 (positive for OMI, using QRS amplitude V2=7.5mm) (> 18.2 is most accurate cutoff; > 19.0 is 97% specific)
This ECG was sent to Pendell, Smith, and Grauer. All immediately diagnosed LAD occlusion.
This ECG pattern as a whole is extremely specific for full thickness, complete ischemia of the anterior, lateral, and inferior/apical walls. There are several etiologies of this (including takotsubo cardiomyopathy, coronary spasm, etc), however the overwhelmingly most likely, most important, and most treatable etiology is acute Occlusion MI (OMI), in this case likely a wraparound LAD that supplies the anterior wall and wraps around to the apex (showing up in the inferior leads). The only way to differentiate OMI from other, less treatable causes is emergent angiogram.
This ECG was interpreted as "no STEMI" and the clinician initiated a typical workup for undifferentiated chest pain.
Approximately an hour or two later, the initial troponin I returned positive at 0.8 ng/mL.
A second ECG was ordered after this troponin resulted:
A third ECG was recorded before transport:
 |
| Similar to prior, ongoing OMI. |
The patient was given ASA, heparin bolus, and thrombolytics. He was transferred to the regional PCI center, and the exact cath outcome was very difficult to obtain, however the findings included triple vessel disease with complicated LAD and LCX lesions that required urgent CABG and balloon pump for cardiogenic shock. The ultimate outcome is not obtainable.
Learning Points:
Never exclude OMI based on age. Young people can have OMI.
You should learn to recognize this pattern of wraparound LAD occlusion, including the subtle but diagnostic hyperacute T-waves in V4 from the original ECG.
This young patient likely would have had a much better outcome if his need for emergent reperfusion had been recognized 1-2 hours earlier.
See these other cases of young people with OMI:
24 yo woman with chest pain: Is this STEMI? Pericarditis? Beware a negative Bedside ultrasound.
See these other similar cases:
The computer and the cardiologist called this a "Normal EKG"
===================================
MY Comment by KEN GRAUER, MD (3/29/2020):
===================================
Sometimes the diagnosis of acute OMI (Occlusion-based MI) will be obvious from the initial ECG. However, much of the time — it won’t be. Achieving 100% certainty that a patient who presents to the ED with new chest pain has acute OMI, and therefore merits prompt cath is simply not a realistic goal in many cases.
- That said — we do not need to be 100% certain. All that should be needed to justify prompt cath for a patient with new chest pain is seeing enough on ECG to consider acute OMI until proven otherwise.
I focus my My Comment in this case on the initial ECG. For clarity — I’ll again show this initial tracing in Figure-1.
- Please take ANOTHER LOOK at this initial ECG ( = ECG #1). Then consider the questions below Figure-1.
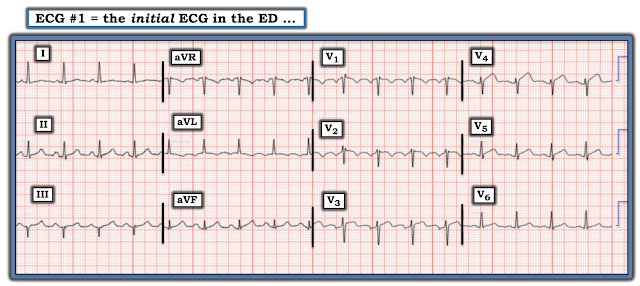 |
| Figure-1: The initial 12-lead ECG in this case (See text). |
QUESTIONS: Given that the patient in this case presented to the ED for new-onset chest pain:
- WHICH ONE of the 12 leads in ECG #1 most concerns you?
- Once you’ve identified the lead with the most worrisome ST-T wave appearance — Are the “neighboring leads” to this most worrisome lead also abnormal?
- Looking at the entire tracing in Figure-1 — HOW MANY of the 12 leads show an abnormal ST-T wave appearance?
- In this patient with new chest pain — Is the sum total of these abnormal leads enough to merit (if not mandate) prompt cardiac catheterization? (ie, After looking at this ECG — Is your diagnosis acute OMI until proven otherwise?).
- EXTRA CREDIT: Which 2 leads in ECG #1 are most likely the result of faulty lead placement? How might this technical mishap affect your decision about whether or not prompt cardiac cath is indicated?
My THOUGHTS: As always — I favor beginning interpretation of ECG #1 with a Systematic Approach:
- The rhythm is sinus tachycardia at a rate just over 100/minute. The PR interval and QRS duration are normal. I suspect the QTc interval is no more than upper normal, though the QTc becomes more difficult to assess with tachycardia, as is seen here. The frontal plane axis is normal (about +20 degrees). There is no chamber enlargement.
Regarding Q-R-S-T Changes:
- There appears to be a large Q wave in lead III — at least, in 3 of the 4 QRS complexes in this lead. Looking closer — there is some beat-to-beat variation in QRS morphology in lead III, with possibly a tiny initial r wave in the 1st complex — and possibly a small terminal r wave in the 2nd and 4th complexes in this lead. Small and narrow q waves appear to be present in at least some beats in multiple leads. That said — I suspect the presence of any Q waves we see on this tracing is not clinically significant.
- R Wave Progression is somewhat delayed (ie, Transition, where the R wave becomes taller than the S wave is deep does not occur until between leads V4-to-V5). NOTE: Recognition that R wave amplitude remains modest as far over as lead V4 in ECG #1 is a relevant finding when contemplating the possibility of acute LAD occlusion (and if anything — R wave amplitude decreases from lead V3-to-lead-V4 in this tracing).
- ST-T Wave Changes in ECG #1 are clearly of concern! — which I address and illustrate in Figure-2 below:
 |
| Figure-2: I’ve labeled ECG #1 to illustrate KEY findings (See text). |
Regarding answers to the QUESTIONS raised above:
- Of the 12 leads in ECG #1 — it is lead V4 that concerns me most. Looking closely — the J-point in lead V4 (BLUE arrow in this lead) is elevated by 2 mm above the PR segment baseline (dotted RED line). As per Dr. Meyers — the ST segment in this lead V4 is straightened (similar to the angled BLUE line in this lead).
- PEARL #1: When assessing less-than-obvious ST-T wave changes in a patient with new-onset symptoms — I have found it helpful to identify at least 1 or 2 leads on the initial 12-lead tracing that are unmistakably abnormal. In this patient with new chest pain — there is NO way the ST-T wave appearance in lead V4 of this tracing should be interpreted as anything but hyperacute until proven otherwise by prompt cardiac catheterization.
- PEARL #2: Support that a clearly abnormal ST-T wave (as we see in lead V4) is indicative of an acute coronary syndrome in progress — can usually be obtained from assessment of “neighboring” leads. We see this in Figure-2 — in which there is ~1 mm of J-point ST elevation with ST segment straightening in both of the leads neighboring lead V4 (angled PURPLE lines in leads V3 and V5).
- PEARL #3: It is almost certain that leads V1 and V2 in ECG #1 have been placed 1 or 2 interspaces too high on the chest because: i) there is an rSr’ appearance in both of these leads; ii) there is a significant negative component to the P wave in both of these leads in this young adult with no apparent reason to have left atrial enlargement; and, iii) the appearance of the QRS complex and the ST-T wave in leads V1 and V2 looks very much like the QRS complex and ST-T wave in lead aVR. (For more on ECG recognition of lead V1,V2 misplacement — Please see My Comment in the November 4, 2018 post).
- KEY: Prompt recognition of lead V1,V2 misplacement is relevant when contemplating possible acute anterior OMI. In this particular case — I would not have needed to immediately repeat ECG #1 — because regardless of what the true ST-T wave appearance in leads V1 and V2 is, definitive ECG findings are already present (as described above) in leads V3, V4 and V5. BUT — 2 more ECGs were obtained on the patient in this case prior to transport — and given persistence of the QRST appearance in leads V1 and V2, it’s obvious that this lead placement error went unrecognized. And, there are times when the ECG diagnosis of acute anterior OMI may depend on availability of an ECG which uses correct placement of leads V1 and V2.
- Finally, as per Dr. Meyers — ST-T wave appearance in the inferior leads, and in lead aVL is clearly abnormal. Although the modest QRS complex amplitude in these leads makes assessment of ST-T wave changes challenging — the T waves in leads III and aVF are hyperacute. Both of these T waves are fatter-at-their-peak and broader-at-their-base than expected — with a T wave that is disproportionately tall (ie, T wave amplitude in lead aVF is almost as tall as the R wave in this lead). Given lack of any appreciable R wave in lead III — the T wave in III is also inappropriately tall. While T wave changes in lead II are more subtle — in the context of clear abnormalities in leads III and aVF, I thought the T wave in lead II was also more prominent than expected. Confirmation that these ST-T wave changes in the inferior leads are real — is forthcoming from the near mirror-image opposite ST-T wave picture that lead aVL manifests compared to the ST-T wave in lead III (ie, there are reciprocal ST-T changes in lead aVL).
BOTTOM LINE Regarding ECG #1: In this patient with new chest pain — acute ST-T wave changes are clearly present in leads II, III, aVF and aVL — and, in leads V3, V4 and V5. I suspect leads V1 and V2 would also show abnormal ST-T waves, if an ECG was repeated with correct lead placement of the V1,V2 electrodes.
- The finding of abnormal ST-T wave changes in at least 7 (if not 9) out of 12 leads on the initial ECG, in this patient with new chest pain — should more than merit justification for prompt cardiac catheterization.
- P.S.: The 2nd ECG in this case was obtained 1 or 2 hours later (after ECG #1). Realizing that “Hindsight is 100% in the Retrospectoscope” — IF there was any doubt after seeing ECG #1 about whether the above noted ECG findings in this patient with new chest pain were acute — then the 2nd ECG in this case should have been obtained much sooner than “1 or 2 hours later”.
Our THANKS to Drs. Fiero and Meyers for sharing this case! There is much to learn from it.















