A 54 yo with history of hypertension awoke in the AM with substernal chest pain. It did not abate, so at 0930, he called 911.
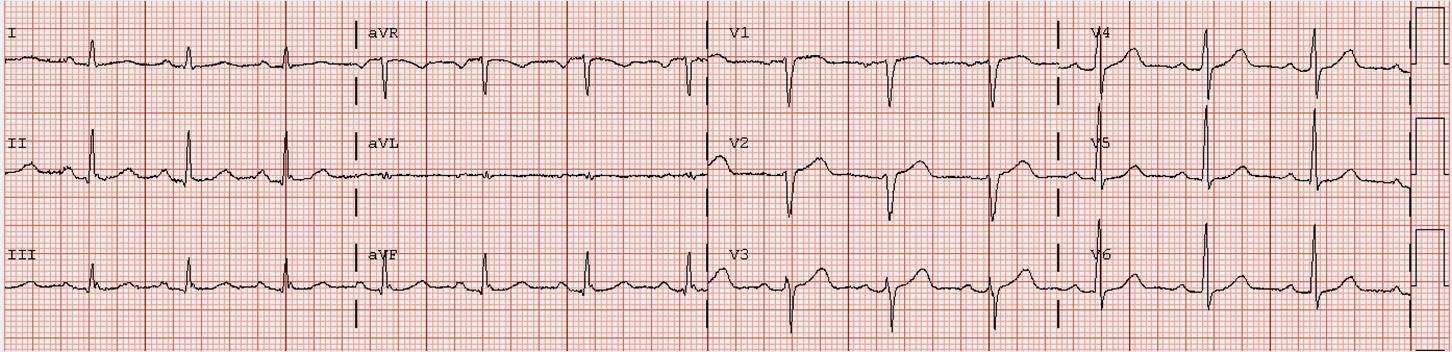
Medics arrived and recorded this ECG:
This is highly suggestive of acute inferolateral STEMI, though not classic. By any millimeter criteria, one would have to call it STEMI. I would call it STEMI but it is not obvious. [Also, tachycardia should always alert you to impending cardiogenic shock, or to possibly another diagnosis such as pulmonary embolism; however, this has none of the other classic findings of PE.]
Our prehospital protocol is:
--If a patient has chest pain and the computer algorithm reads ***Acute MI***, then they are to activate the cath lab from the field.
--If only one of these is present, they are not to do so.
The computer algorithm made no comment on any of it.
Fortunately, our medics sometimes go outside the rules. That is what they did here: activate the cath lab.
The patient arrived in the ED at 1022 and had this ECG recorded at 1028:
The patient was taken to the cath lab at 1039. As he was being transferred to the cath table he had a v fib arrest. He was defibrillated. Angiogram showed a type III (wraparound) LAD, occluded distally (but also with an 80% diagonal stenosis), such that he was having an infero-antero-apical STEMI. The thrombosis was opened, thrombus suctioned, and the lesion stented, with a door to balloon time of 45 minutes (thanks to prehospital activation by the medics).
Medics are getting very good at reading the ECG; maybe it is time to let them overrule the computer? --This requires a formal study.
General methods:
Take one or more EMS service(s) in which medics are well trained in reading the 12-lead. Search for all patients who had a prehospital ECG. Find the cath outcome, or troponin outcome if no MI. Find the computer read on the ECG. Have 2-4 medics read the ECG blinded to the computer and the outcome. Compare.
Medics arrived and recorded this ECG:
Our prehospital protocol is:
--If a patient has chest pain and the computer algorithm reads ***Acute MI***, then they are to activate the cath lab from the field.
--If only one of these is present, they are not to do so.
The computer algorithm made no comment on any of it.
Fortunately, our medics sometimes go outside the rules. That is what they did here: activate the cath lab.
The patient arrived in the ED at 1022 and had this ECG recorded at 1028:
 | |
|
The patient was taken to the cath lab at 1039. As he was being transferred to the cath table he had a v fib arrest. He was defibrillated. Angiogram showed a type III (wraparound) LAD, occluded distally (but also with an 80% diagonal stenosis), such that he was having an infero-antero-apical STEMI. The thrombosis was opened, thrombus suctioned, and the lesion stented, with a door to balloon time of 45 minutes (thanks to prehospital activation by the medics).
Medics are getting very good at reading the ECG; maybe it is time to let them overrule the computer? --This requires a formal study.
General methods:
Take one or more EMS service(s) in which medics are well trained in reading the 12-lead. Search for all patients who had a prehospital ECG. Find the cath outcome, or troponin outcome if no MI. Find the computer read on the ECG. Have 2-4 medics read the ECG blinded to the computer and the outcome. Compare.