A 50-something male presented to a clinic for one day of intermittent substernal chest and jaw pain. He had had several episodes of pain since onset; it was described as pressure-like and lasts about 5-15 minutes and resolves spontaneously. He had been pain free for about an hour. He had some "pre-diabetes," but no h/o hypertension, no known family history of heart disease, and he smokes about 1-2 cigarettes per day.
An ECG was recorded:
 |
| The computer read: Normal ECG What do you think? Veritas algorithm |
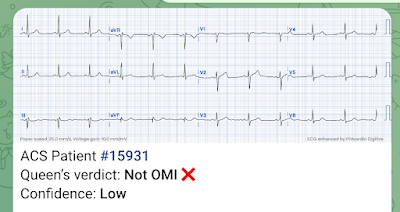
I sent this to the Queen years later. You can see that she does not see OMI, but she has low confidence. In other words, she would never call this "normal."
The Queen of Hearts PM Cardio App is now available in the European Union (CE approved) the App Store and on Google Play. For Americans, you need to wait for the FDA. But in the meantime:
YOU HAVE THE OPPORTUNITY TO GET EARLY ACCESS TO THE PM Cardio AI BOT!! (THE PM CARDIO OMI AI APP)
If you want this bot to help you make the early diagnosis of OMI and save your patient and his/her myocardium, you can sign up to get an early beta version of the bot here. It is not yet available, but this is your way to get on the list.
Smith Comment:
This is definitely not a normal ECG.
There is less than 1 mm of ST depression in II, III, aVF, and in V3-V6.
The STD is nearly 1 mm in III and V6.
There is a tiny amount of ST Elevation in aVL
The ST vector is around -60 degrees, so that there is some STE in aVL and a bit in I, and zero in aVR
What is a normal ST segment?
--First, one must be sure that the QRS is normal. An abnormal QRS (abnormal depolarization), such as in LBBB, LVH, RBBB, or RVH, may result in abnormal ST-T (abnormal repolarization). In this case, the QRS is normal: normal axis, duration, and amplitude, without abnormal Q-waves.
When the QRS is normal
--The normal ST vector is towards leads II and V5 (anterior and leftward)
--Leads I, II, and aVF should not have any ST depression, as the normal ST vector is leftward and anterior. It is common to have some normal variant ST elevation in these leads, often called "early repolarization."
--Precordial leads also usually have normal ST elevation, not ST depression.
--Up to 0.5 mm of ST depression can be normal, though it is unusual. It should not be assumed to be normal unless there are previous ECGs that confirm it.
Causes of ST Depression with a normal QRS:
1. Normal Variant
2. Ischemia
3. Hypokalemia
4. Digoxin
It is very likely that the "inferior ST depression" is due to high lateral MI. The ST depression in precordial leads suggest still more widespread ischemia, so the exact culprit is not at all clear.
Case continued
He was diagnosed with reflux and treated with a proton pump inhibitor and given nitroglycerin.
He presented to the ED 1 day later:
He stated that he had continued episodes of chest pain and then it became constant that morning (about 8 hours prior). The NTG had not helped. There is no change in symptoms with exertion, the pain is not pleuritic, positional, or reproducible by palpation.
An ECG was recorded:
Here is yesterday's for direct comparison:
The patient was given aspirin and his first troponin returned at 4.94 ng/mL. The pain spontaneously resolved. He was given heparin and metoprolol, with a plan to go urgently to cath if his pain recurred.
Another ECG was recorded at t = 46 minutes:
 |
| There is less ST depression |
This was recorded at T = 105 minutes
 |
| There is a suggestion of terminal T-wave inversion in V2, suggestive of Wellens' waves |
The next AM, this was recorded before the angiogram:
 |
| What is the culprit artery? |
Here is the troponin profile:
The angiogram showed a 100% thrombotic mid-LAD occlusion with faint left to right and right to left collaterals.
Here is the post cath ECG:
So that very subtle terminal T-wave inversion were indeed subtle Wellens' waves.
In Wellens' original studies, every case had either an open artery (LAD) or collateral circulation. Wellens' waves imply reperfusion, but it might be due to collaterals, not due to reperfusion of the infarct-related artery.
Learning Points
1. Beware ST depression
2. Never assume chest pain is reflux. They cannot be differentiated without troponin. (The ECG could be entirely normal in MI, though in this case it was NOT normal)
3. Wellens' syndrome is due to reperfusion or good collateral circulation
4. Ischemia that resolves need not go to the cath lab emergently as long as there is very close monitoring.
See this case: