This patient was found down in a Minneapolis winter. He was very cold with frostbitten fingers and toes. He was alert but encephalopathic and delirious and very agitated and could not be adequately calmed with olanzapine and lorazepam, so we intubated him. The first reliable temperature could only be obtained with a Foley thermistor, and it was 26.5 degrees C (79.7 F).
His BP was 76/60. K was 2.8 mEq/L.
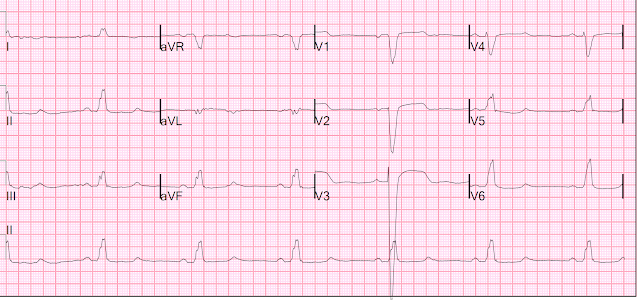
Here was his first ECG:
In general, it is probably best to NOT correct the QT when the heart rate is below 60. (See this article by Megan Rischall and me). If one did correct for a heart rate of 41, one would get 661 by Bazett and 767 by Hodges.
LBBB QT interval is distorted by the QRS duration. To compensate, there are a number of methods to correct for the QT in LBBB.
The patient did not require ECMO, as many of our Northland hypothermia patients do, because he did not meet our protocol guidelines: his temp was not below 24C, it was between 24 and 28 with stable hemodynamics (BP of 75 systolic is excellent for someone with a temp from 24-28), and he did not have frozen extremities (hands/feet/arms legs) -- fingers and toes alone do not count.
But he did require internal rewarming (external rewarming is contraindicated, as it can cause either or both of rewarming shock or core afterdrop -- see below), which can be done with an intravenous warming catheter with or without adjunctive gastric, bladder, intraperitoneal, and/or intrathoracic rewarming. We placed an intravenous warming catheter (Zoll, Alsius Coolgard) and added bladder and gastric rewarming since he was so stable.
He was also found to have pneumonia and treated with antibiotics.
He slowly rewarmed, and had these subsequent ECGs
2nd, at 5 hours and 29.6 degrees:
3rd ECG at 8 hours and 32.5 degrees:
The next AM he was actually febrile, and had this ECG:
Learning Points:
1. Hypothermia results in appropriate bradycardia and hypotension
2. Severe hypothermia should be rewarmed internally
3. The QT is prolonged in hypothermia
4. The QT interval is artifactually prolonged in LBBB by the QRS duration
5. To correct for QRS prolongation, QT in LBBB can be measured with the Tpeak to Tend interval, and this interval is often also corrected for heart rate.
The best review article on Accidental Hypothermia
--written by my partners Megan Rischall and Andie Rowland-Fischer.
Full text: Evidence-Based Management Of Accidental Hypothermia In The Emergency Department
Excerpts:
Electrocardiography in Hypothermia
J waves, also called Osborn waves, are a well-known ECG abnormality in hypothermic patients. J waves manifest as positive deflection at the termination of the QRS complex with associated J-point elevation. (See Figure). They are generally present when core temperature is below 32°C, and their size is inversely related to core temperature.27 Multiple observational studies, including a total of 150 patients with accidental hypothermia, showed that J waves were present in all patients whose body temperature was below 30°C.30 J waves are expected to get smaller with rewarming, but they can persist even after normothermia is achieved. Although they are most commonly associated with hypothermia, J waves have been described in patients with subarachnoid hemorrhage, acute cardiac ischemia, and in normothermic patients. In mild hypothermia, sinus rhythm predominates. In moderate hypothermia, atrial fibrillation with slow ventricular response becomes the most common rhythm, but sinus bradycardia, atrial reentrant rhythms, and junctional rhythms can also be seen. Myocardial irritability may manifest with ectopic ventricular beats. As hypothermia becomes more severe, the risk of ventricular fibrillation and asystole increases. In moderate and severe hypothermia, slowing of the myocardial conduction, depolarization, and repolarization can result in PR prolongation, atrioventricular block, QRS widening and QTc prolongation.
Smith ECG Blog posts of Osborn waves
--Massive Osborn Waves of Severe Hypothermia (23.6 C), with Cardiac Echo
--Osborn Waves and Hypothermia (this is the "Figure" above)
Rewarming Shock and Core Afterdrop:
Caution must be taken when using active external rewarming. Peripheral vasoconstriction makes the skin more susceptible to thermal injures, and there have been case reports of full thickness burns from both warm chemical packs and forced air heating systems.47 In moderately and severely hypothermic patients, the emergency clinician should also take care to rewarm a patient’s trunk prior to warming the extremities. Rewarming the extremities reverses peripheral vasoconstriction and cooled, acidemic blood that is pooled in the extremities returns to the core, potentially causing further drop in core temperature and pH, called core afterdrop. Additionally, peripheral vasodilation increases intravascular space, pulling blood away from central circulation, potentially leading to hemodynamic instability and sometimes resulting in ventricular fibrillation. This phenomenon is discussed further in the “Controversies.”
Controversies
Core Afterdrop
There is much discussion surrounding the phenomenon of core afterdrop, which is the decrease in core temperature secondary to increasing blood flow to cold extremities. This causes the return of cold, acidemic blood to central circulation, in turn causing further drop in core temperature and worsening acidosis. Peripheral vasodilation also contributes to hemodynamic instability, and all of these factors put the patient at increased risk of fatal dysrhythmias during the rewarming process. Patients with moderate-to-severe hypothermia are particularly sensitive to even a small temperature drop, and this can lead to circulatory collapse.
The etiology, severity, and clinical significance of core afterdrop have been debated. Some believe that core afterdrop is caused by active external rewarming, and, more specifically, rewarming the extremities in conjunction with the core. Others suggest that core afterdrop is inevitable regardless of rewarming method, as temperature will temporarily decrease in any object with a warm core and cool periphery, due to conductive properties.73 Studies on afterdrop are conflicting, and this is an area in need of further research. In the meantime, we recommend initially limiting the movement or warming of extremities so as to limit the potential for an afterdrop effect.
Additional information from UpToDate on External Rewarming of Severe Accidental Hypothermia:
Active external rewarming — During active external rewarming, some combination of warm blankets, heating pads, radiant heat, warm baths, or forced warm air is applied directly to the patient's skin. These methods are indicated for moderate to severe hypothermia (<32°C) and for patients with mild hypothermia who lack physiologic reserve or fail to respond to passive external rewarming. Active external rewarming provides an effective initial strategy for most spontaneously perfusing, severely hypothermic patients.
Especially in chronic hypothermia with dehydration, rewarming of the trunk should be undertaken before the extremities. These actions are performed in order to minimize core temperature afterdrop with associated hypotension and acidemia due to arterial vasodilation [22,24,80]. With forced air warming systems, the extremities can be left uncovered initially. This minimizes afterdrop but allows heat transfer.
Hazardous core temperature afterdrop is a particular risk of active external rewarming. This complication occurs when the extremities and trunk are warmed simultaneously. Cold, acidemic blood that has pooled in the vasoconstricted extremities of the hypothermic patient returns to the core circulation, causing a drop in temperature and pH. At the same time, removal from the cold environment results in peripheral vasodilation, potentially contributing to precipitous hypotension, inadequate coronary perfusion, and ventricular fibrillation [10]. These phenomena may explain the fatal dysrhythmias that sometimes occur during rewarming [81,82]. Combining active core rewarming techniques with active external rewarming can minimize rewarming shock and afterdrop in patients with severe hypothermia [83] (see 'Active internal (core) rewarming' below). However, there is no evidence that prehospital external rewarming is dangerous for patients with accidental hypothermia [84].




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.