This is another case provided by Mustafa Alwan, an internist from Jordan and very talented ECG enthusiast. He posted it on Facebook EKG Club, and I am reposting with his permission.
Case
This is a 26 year old male who presented after having had 2 episodes of syncope in 1 day. Both episodes started with palpitations, then dizziness. He had no family history of sudden death.
Vital signs: normal
Initial ECG :
See this post for a review of Type 2 Brugada.
The method is to draw a line from the peak of the R'-wave down along the downslope of the R'-wave, as shown. At a point which is 5 mm below the peak, you draw a line across and if the distance to the S-wave is greater than 3.5 mm, it is a wide beta angle. This is equivalent to a 35 degree angle, or 0.61 radians (calculated as the inverse tangent of 3.5/5, or 0.7).
Dr. Ken Grauer, the ECG master who runs this site: http://ecg-interpretation.blogspot.com/, measured the beta angle here:
For those wanting more — go to minute 21:19 in Ken's ECG Video on Brugada Syndrome. Here is the link to this specific point in the video — https://youtu.be/h1MhtLMF-7M?t=21m19s
Type 2 Brugada morphology (in contrast to syndrome) is really quite common, and if you rely on the morphology alone, without the other criteria for syndrome (see below), you will have a lot of false positives.
Diagnosis of Brugada Syndrome requires both:
1. Brugada pattern ECG (either Brugada Type 1, or the newly defined Brugada Type 2 morphology)
Findings may be dynamic and are sometimes concealed; findings may be observed only in certain circumstances such as fever, intoxication, electrolyte imbalance, presence of sodium channel medications/drugs, or vagal stimulation.
2. At least one of the following:
(a) survivor of cardiac arrest,
(b) witnessed/recorded polymorphic ventricular tachycardia (VT),
(c) history of nonvagal syncope,
(d) familial antecedents of sudden death in patients younger than 45 years without acute coronary
syndrome
(e) Type 1 Brugada pattern in relatives.
This patient only had (c), and no other criteria.
So this ECG did not even meet the criteria for Type 2 Brugada morphology (because the beta angle was too small). These criteria were developed in a comparison of Brugada syndrome patients with athletes who have an Rsr' saddleback, and they were about 90% sensitive and 90% specific, so they weren't perfect.
Presumably because this patient had 2 episodes of non-vagal syncope, he was admitted for observation and the admitting cardiologist referred him for Ajmaline challenge test (a sodium channel blocker) in the electrophysiology (EP) lab.
Here is the resulting ECG:
Commentary
Does this establish Brugada syndrome?
One cannot clearly state that there is, or is not, Brugada syndrome due to response to Ajmaline or other Na channel blockers. One can only risk stratify for future arrhythmic events.
The considerations for ICD implantation are far beyond the scope of this article and all such patients should be evaulated by an electrophysiologist.
Not all emergency and primary care physicians, and even some general cardiologists, recognize these important issues:
This paper (full text) discusses the risk of arrhythmia in patients who have spontaneous vs. drug induced (e.g. ajmaline) type 1 morphology. If the patient only has a history of syncope (like our patient), the risk of future arrhythmic events is 0.6%-1.9%. If the patient with only drug-induced Brugada morphology is asymptomatic (unlike this patient), the risk of future arrhythmia is extremely low.
They reference this paper which shows that ICD implantation has a high rate of inappropriate shock and that the ICD's record a low annual rate of dysrhythmia.
Moreover, the authors of this study, (Outcome After Implantation of a Cardioverter-Defibrillator in Patients With Brugada Syndrome) found that the best cutoff for the beta angle is wider than 35 degrees. It is 58 degrees, which corresponds to a triangle base width of 8 mm (not 3.5 mm!!).
Here are the latest recommendations from this 2014 publication (full text: HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes):
Here are the full recommendations:
Case
This is a 26 year old male who presented after having had 2 episodes of syncope in 1 day. Both episodes started with palpitations, then dizziness. He had no family history of sudden death.
Vital signs: normal
Initial ECG :
 |
| This is suggestive of Type 2 Brugada morphology because of the Saddleback in lead V2 At first glance, the beta angle looks wide. |
The method is to draw a line from the peak of the R'-wave down along the downslope of the R'-wave, as shown. At a point which is 5 mm below the peak, you draw a line across and if the distance to the S-wave is greater than 3.5 mm, it is a wide beta angle. This is equivalent to a 35 degree angle, or 0.61 radians (calculated as the inverse tangent of 3.5/5, or 0.7).
Dr. Ken Grauer, the ECG master who runs this site: http://ecg-interpretation.blogspot.com/, measured the beta angle here:
 |
| So the beta angle is not wide enough to meet type 2 Brugada morphology criteria |
For those wanting more — go to minute 21:19 in Ken's ECG Video on Brugada Syndrome. Here is the link to this specific point in the video — https://youtu.be/
Type 2 Brugada morphology (in contrast to syndrome) is really quite common, and if you rely on the morphology alone, without the other criteria for syndrome (see below), you will have a lot of false positives.
Diagnosis of Brugada Syndrome requires both:
1. Brugada pattern ECG (either Brugada Type 1, or the newly defined Brugada Type 2 morphology)
Findings may be dynamic and are sometimes concealed; findings may be observed only in certain circumstances such as fever, intoxication, electrolyte imbalance, presence of sodium channel medications/drugs, or vagal stimulation.
2. At least one of the following:
(a) survivor of cardiac arrest,
(b) witnessed/recorded polymorphic ventricular tachycardia (VT),
(c) history of nonvagal syncope,
(d) familial antecedents of sudden death in patients younger than 45 years without acute coronary
syndrome
(e) Type 1 Brugada pattern in relatives.
This patient only had (c), and no other criteria.
So this ECG did not even meet the criteria for Type 2 Brugada morphology (because the beta angle was too small). These criteria were developed in a comparison of Brugada syndrome patients with athletes who have an Rsr' saddleback, and they were about 90% sensitive and 90% specific, so they weren't perfect.
Presumably because this patient had 2 episodes of non-vagal syncope, he was admitted for observation and the admitting cardiologist referred him for Ajmaline challenge test (a sodium channel blocker) in the electrophysiology (EP) lab.
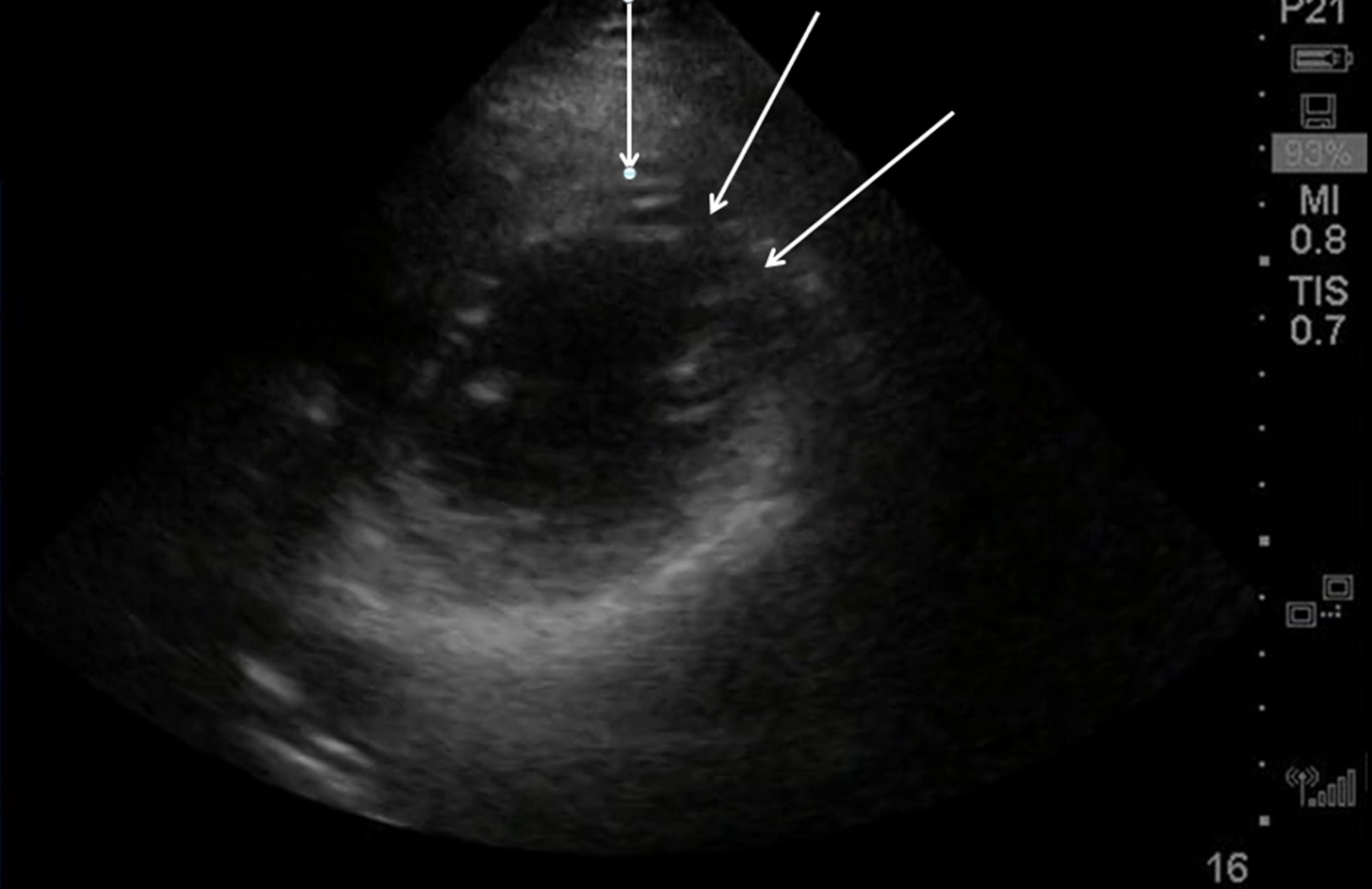
Here is the resulting ECG:
 |
| Now there is clearly Brugada morphology. |
Commentary
Does this establish Brugada syndrome?
One cannot clearly state that there is, or is not, Brugada syndrome due to response to Ajmaline or other Na channel blockers. One can only risk stratify for future arrhythmic events.
The considerations for ICD implantation are far beyond the scope of this article and all such patients should be evaulated by an electrophysiologist.
Not all emergency and primary care physicians, and even some general cardiologists, recognize these important issues:
This paper (full text) discusses the risk of arrhythmia in patients who have spontaneous vs. drug induced (e.g. ajmaline) type 1 morphology. If the patient only has a history of syncope (like our patient), the risk of future arrhythmic events is 0.6%-1.9%. If the patient with only drug-induced Brugada morphology is asymptomatic (unlike this patient), the risk of future arrhythmia is extremely low.
They reference this paper which shows that ICD implantation has a high rate of inappropriate shock and that the ICD's record a low annual rate of dysrhythmia.
Moreover, the authors of this study, (Outcome After Implantation of a Cardioverter-Defibrillator in Patients With Brugada Syndrome) found that the best cutoff for the beta angle is wider than 35 degrees. It is 58 degrees, which corresponds to a triangle base width of 8 mm (not 3.5 mm!!).
Here are the latest recommendations from this 2014 publication (full text: HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes):
 |
| Unfortunately, the situation of our patient is not reflected here: Symptomatic with drug induced Type 1 ECG, but no family history |
Here are the full recommendations:
| Class I | |
| |
| Class IIa | |
| |
| Class IIb | |
| |
| Class III | |
|