Written by Pendell Meyers
A woman in her 70s with known prior coronary artery disease experienced acute chest pain and shortness of breath. The chest pain was described as severe pressure radiating to both shoulders. Vital signs were within normal limits.
She presented to the Emergency Department at around 3.5 hours since onset. She had taken aspirin at home.
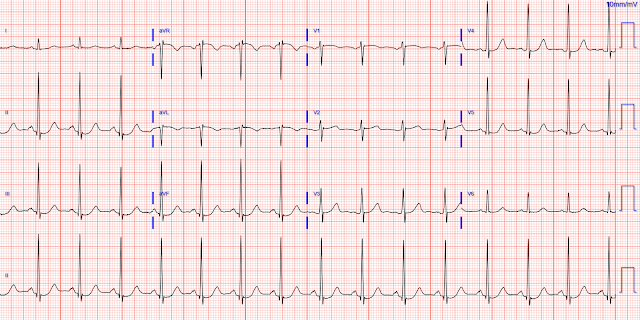
Here is her triage ECG:
 |
| What do you think? |
The ECG shows sinus rhythm with normal QRS complex morphology and significant subendocardial ischemia (SEI) pattern (ST depression in many leads, worst in lateral areas including leads II, V5-6, with reciprocal STE in aVR). One could argue or wonder if there is both subendocardial ischemia AND posterior OMI pattern, since the STD in V4 may be equal or possibly slightly worse proportionally than V6.
But thankfully, when the clinical context is clearly and highly concerning for ongoing ischemia from ACS, this distinction doesn't matter much. Whether an ECG shows a pattern of OMI, SEI, both, or neither, the patient with ongoing ischemia needs to be considered for emergent reperfusion therapy.
The Queen of Hearts is totally blinded to clinical context, and an upcoming model (that can independently report OMI vs SEI) identified SEI with high confidence.
While it is not necessary to have a prior baseline ECG in this case, there was one available:
 |
| Within normal limits. |
 |
| Pre-intervention. |
 |
| Post-intervention. |
Here is her ECG within 30 minutes of PCI:
 |
| Improved, but still with ischemia. |
 |
| Almost back to normal. |
High sensitivity Troponin I:
(prior baseline within normal limit)
185 ng/L
638 ng/L
13,916 ng/L
(none further measured)
Echo:
EF 45%, hypokinesis of the inferior wall and basal to mid posterolateral segments.
Final Diagnosis: "STEMI" (of course, as you can see in the ECGs above, this is not true, by definition this was NSTEMI. But the "final diagnosis" commonly just reflects whether the patient was given emergent therapy or not, regardless of the definition of STEMI/NSTEMI).
In other words, millimeters really don't matter!
Smith: This SEI pattern is one of global subendocardial ischemia, not of transmural ischemia. The ST depression vector is towards lead II, so the STE vector is towards aVR. This STE in aVR is NOT analogous to STE of STEMI/OMI because there is no ventricular wall that corresponds to aVR--there are only atria on the top (or "base") of the heart. This STE is RECIPROCAL STE, reciprocal to the ST depression.
This SEI pattern is often attributed to "Left Main Occlusion". This idea is erroneous. Patients with complete left main occlusion usually die before arrival in the ED. When they do not die, there are a variety of ECG patterns, shown in the post below. This pattern is indeed consistent with left main ischemia (artery open but with insufficient flow), but it is also consistent with subtotal LAD ischemia and even with a culprit in any of the 3 epicardial vessels in addition to stenosis in the others ("3 vessel ACS").
Additionally, if we had an ECG recorded during complete occlusion of the circumflex with TIMI-0 flow, it would likely show Aslanger's pattern, which is inferior OMI plus SEI simultaneously. With SEI alone, the ST depression vector would be towards lead II (so the STE vector is towards aVR), but with circ occlusion, there would also be an STE vector towards lead III. The combined vector is exactly to the right, such that the only leads with STE are III and aVR. These are not "consecutive" leads, so there is only a single lead with STE and it often does not meet 1 mm.
The pattern is defined as:
(1) any STE in lead III but not in other inferior leads,
(2) STD in any of leads V4 to V6 (but not in V2) with a positive or terminally positive T-wave,
(3) ST in lead V1 higher than ST in V2
This figure shows the ST vector in Aslanger's:
See this post for 8 cases of total Left Main Occlusion: How does Acute Total Left Main Coronary occlusion present on the ECG?
See what happens when a left main thrombus evolves from subtotal occlusion to total occlusion.
MY Comment, by KEN GRAUER, MD (12/31/2024):
- The patient is an older woman with known coronary disease — who presents with severe CP (Chest Pain) of 3.5 hours duration.
- As per Dr. Meyers — the patient's initial ECG (TOP tracing in Figure-1) — shows sinus rhythm — diffuse ST depression (seen here in 8/12 leads) with ST elevation in lead aVR > V1 (RED arrows in aVR, V1).
- Category #1: Severe Coronary Disease (due to LMain, proximal LAD, and/or severe 2- or 3-vessel disease) — which in the right clinical context may indicate ACS (Acute Coronary Syndrome).
- Category #2: Subendocardial Ischemia from some other Cause (ie, sustained tachycardia — be this sinus tachycardia or some other arrhythmia; shock or profound hypotension; respiratory failure; GI bleeding; anemia, "sick patient", etc.).
- DSI does not indicate acute coronary occlusion! While true that many patients with DSI do have severe coronary disease — they generally do not have acute coronary occlusion at the time they are seen (although today's case illustrates a patient who developed acute coronary occlusion after ECG #1 was recorded, during the time that cardiac catheterization was being performed).
- That said, depending on the clinical setting — a significant number of patients who present with the ECG picture of DSI will turn out not to have coronary disease as the cause.
- In today's case, given that the patient was an older woman with known coronary disease — who presented with new CP — severe coronary disease (ie, Category #1) was almost certain to be the cause of the DSI pattern that we see in ECG #1.
- In contrast, despite the pattern of DSI seen in the BOTTOM tracing in Figure-1 (ie, with diffuse ST depression and ST elevation in aVR>V1) — entities other than coronary disease that are listed under Category #2 should be strongly considered because of the tachycardia! This ECG is taken from the July 25, 2024 post in Dr. Smith's ECG Blog. The patient was a younger adult with drug overdose and respiratory arrest, leading to the sinus tachycardia that we see in this bottom tracing (PINK arrows highlighting sinus P waves in other leads — because the fast rate rendered lead II P waves difficult to identify).
- The ECG pattern of DSI is usually easy to recognize — because in a supraventricular rhythm, there is diffuse ST depression (generally in at least 6 leads — often most prominent in lateral chest leads) — in association with ST elevation in lead aVR>V1.
- This pattern of DSI does not mean there is acute coronary occlusion.
- Many (but not all) patients with DSI have severe coronary disease.
- The presence of tachycardia in association with the ECG pattern of DSI serves as a clue that rather than severe coronary disease — one or more of the entities listed above in Category #2 may be the cause.
- And, as per Dr. Smith above — ST elevation in lead III (but not in other inferior leads) — in association with a pattern that is otherwise consistent with DSI — suggests Aslanger's pattern, in which there is inferior OMI plus severe disease in other coronary vessels.
-USE.png) |
| Figure-1: Comparison between the initial ECG in today's case — with the ECG shown in the July 25, 2024 post (See text). |

-mislabelled.png)








-USE.png)








-USE.png)





-USE.png)