This case comes from Jesse McLaren, with some contribution by Smith.
Dr McLaren (@https://twitter.com/ECGcases), is an Emergency Physician in Toronto with a special interest in emergency cardiology quality improvement and education. He is an Assistant Professor at the University of Toronto.
2 Cases
Two patients presented with chest pain. How would you interpret their ECGs, and which had the more myocardial damage?
Patient 1: 55yo with 5 days of intermittent chest pain, now constant. Normal vitals.
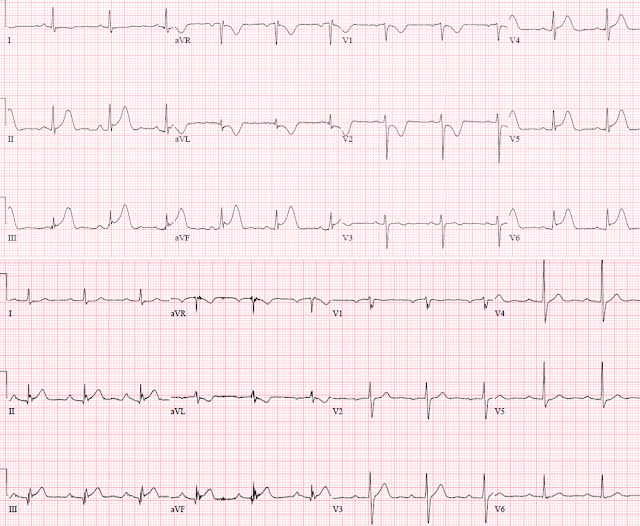
Old, baseline, ECG
There is normal sinus rhythm, normal conduction, normal conduction, normal R wave progression and normal voltages. There is concave ST elevation in all three inferior leads meeting STEMI criteria, along with hyperacute T waves and reciprocal ST depression and T wave in inversion in aVL; ST depression and T wave inversion in V1-2 from posterior MI, and ST elevation and hyperacute T waves in V5-6 from lateral MI.
This is an obvious infero-postero-lateral STEMI (+) OMI, identified by the machine and recognized by the emergency physician. The patient was treated with dual antiplatelets, heparin and nitro, and the cath lab was activated.
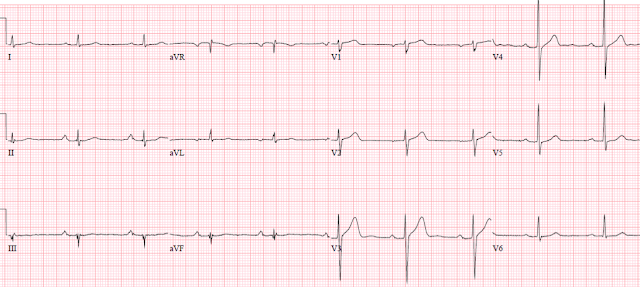
Two minutes later the chest pain resolved and the ECG was repeated:
This ECG, if it had been recorded in isolation, would be highly suspicious for acute ischemia, but not OMI
There is resolution of the inferolateral ST elevation but residual reciprocal ST depression in aVL, and mild precordial ST depression.
Despite having a transient Occlusion, with ST segments that meet STEMI criteria, the patient was still sent to the cath lab, and before the procedure had another episode of chest pain with recurrence of infero-postero-lateral STEMI(+)OMI ECG:
On angiogram there was a 99% circumflex occlusion, but with TIMI-3 flow, which was stented. All troponins were completely normal, at 2 ng/L, just above the limit of detection (LoD). (Abbott Alinity high sensitivity troponin assay, LoD = 1.6 ng/L; URL = 26 ng/L for men, 16 ng/L for women).
Notice that we never called this a "STEMI" because it never actually met the definition of acute MI!!
The definition of MI requires at least one elevated troponin, so the patient actually "ruled out" for acute MI!
Post cath ECG:
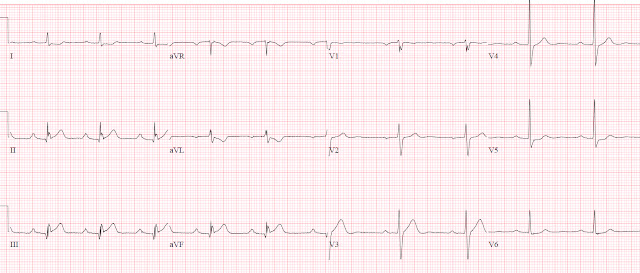
Patient 2: 65yo with 30 minutes of chest pain and normal vitals. Old then new ECG:
There is normal sinus rhythm, with 1st degree AV block and otherwise normal conduction, normal axis, normal R wave progression, normal voltages.
Compared to prior there is subtle concave inferior ST elevation which does not meet STEMI criteria. But there are also inferior hyperacute T waves (large relative to the QRS complex and compared to baseline), and there is new primary reciprocal ST depression and T wave inversion in aVL, which is highly sensitive for inferior OMI. There may also be some pseudonormalization of the ST segment in V2 from posterior MI.
Despite being STEMI negative and labeled normal by the machine, the physician was concerned so gave aspirin and the ECG was repeated 20 minutes after the first:
ECG is similar and patient had ongoing pain. Treated with dual antiplatelets, heparin and cath lab activation: 100% mid RCA occlusion. First trop 26 (borderline normal) and peak 55,000, with inferior basal hypokinesis.
A peak troponin I of 55,000 ng/L is a level that is associated with very large acute MI (lots of myocardial loss).
Discharge ECG:
Discussion
According to the current paradigm based on ECG millimeter criteria, the first patient had STEMI requiring emergent reperfusion while the second did not have STEMI so could have been treated with delayed reperfusion. But the second patient had a totally occluded artery leading to a large MI despite rapid reperfusion, and admitting them as “NSTEMI” with next day angiography could have been fatal. According to the discharge summaries, which seemed to be based on culprit lesions that received rapid reperfusion, both patients had “STEMI” despite the first never having a rise in troponin and the second not meeting STEMI criteria.
We need to start with the underlying pathology. Both patients presented to the ED with Occlusion MI, i.e. “acute occlusion or near occlusion of a major epicardial coronary vessel with insufficient collateral circulation, resulting in imminent necrosis of downstream myocardium without emergent reperfusion.” Both patients also had ECGs diagnostic of OMI on ED presentation: rather than falsely separating these ECGs into STEMI vs NSTEMI based on ST elevation millimeter criteria, we can see that they both had some degree of inferior ST elevation along with hyperacute T waves and reciprocal change in aVL. Both STEMI(+)OMI and STEMI(-)OMI have similar clinical, laboratory and echocardiographic features.
These cases had different outcomes, not based on which met STEMI criteria, but based on which OMI had rapid reperfusion.
The first patient presented with STEMI(+)OMI but had such rapid spontaneous reperfusion, followed by angiography, that they avoided myocardial necrosis completely—without a rise in troponin or ECG evidence of infarction or reperfusion. (But if this “transient STEMI” had not had rapid cath lab activation, they might have re-occluded and developed a preventable infarct).
In fact, this case does not even meet the formal definition of myocardial infarction (!), by the 4th Universal Definition, which requires a rise and fall of troponin with one value above the 99th percentiile. It is, in fact, ST Elevation Unstable Angina. Had the patient had ECGs recorded at different moments, this would have been entirely missed
The second patient presented with STEMI(-)OMI but had a total occlusion that persisted despite initial management and was only relieved in the cath lab—with a resulting significant rise in troponin despite rapid diagnosis, and ECG evidence of infarction and reperfusion. Instead of these patients both having a discharge diagnosis of “STEMI”, the first had unstable angina from “OMI that is so brief or so quickly treated that troponins do not rise, MI prevented”, while the second had STEMI(-)OMI.
Take home
1. Automated interpretation is unreliable, even those labeled “normal”
2. STEMI criteria has poor sensitivity for Occlusion MI
3. Primary reciprocal ST depression in aVL is highly sensitive for inferior OMI, and can highlight subtle inferior ST elevation and hyperacute T waves
4. Acute coronary occlusion is a dynamic process that can spontaneously reperfuse and reocclude, and "transient STEMIs" are at risk for reocclusion
5. Initial troponins are unreliable for STEMI/OMI, and serial troponins can miss unstable angina from transient occlusions
6.
MIs
should be classified based on the underlying pathology of OMI/NOMI, not
STEMI/NSTEMI criteria, and this should be reflected in the discharge diagnosis to accurately track and learn from cases
References
1. Bischof et al. ST depression in aVL differentiates inferior ST-elevation myocardial infarction from pericarditis. Am J Emerg Med 2016
2. Meyers et al. Comparison of the ST-elevation myocardial infarction (STEMI) vs NSTEMI and Occlusion MI (OMI) vs NOMI paradigms of acute MI. J of Emerg Med 2021









No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.