60-something with h/o MI and stents presented with chest pain radiating to the back and nausea/vomiting.
Time zero
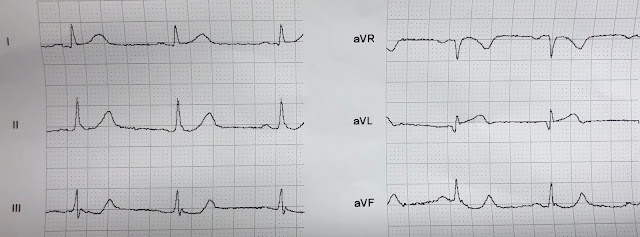
There is inferior ST elevation. Is it normal variant? Is it ischemic (OMI)? [Pericarditis? (NOT!)]
There is one finding that argues against inferior OMI (There is absence of reciprocal ST depression in aVL; STD aVL is extremely sensitive for inferior OMI; Reference: Bischof and Smith).
However, there is also straightening of the inferior ST segments, and a straight ST segment in aVF; this is extremely rare in normal variant STE).
_______
There is also terminal QRS distortion in II, III, aVF [absence of S-wave and J-wave (notch)]. The significance of this in inferior leads is unknown, but I suspect it is a marker for inferior OMI vs. normal variant.
Terminal QRS distortion is definitely significant for anterior OMI in V2 and V3:
Here is an ECG from one month ago:
The patient was given aspirin, heparin, and IV nitroglycerine.
Another ECG was recorded at 35 minutes:
At this point, the first troponin I returned at 0.55 ng/mL (significantly elevated)
A D dimer was also elevated.
Another ECG was recorded at 58 minutes:
There was concern for aortic dissection, so a CT was done and was negative.
The cath lab was activated:
Formal Echo:
Learning Points:
1. Any inferior ST elevation may be acute OMI, but there are subtle differences between OMI on the one hand, and normal variant on the other.
2. 99% of inferior OMI are either obvious or have some amount of ST depression in aVL. But 1% may be/have neither!
3. In this case, one might say it is "obvious" MI because of a straight ST segment in aVF. A straight ST segment virtually never happens in inferior ST elevation that is NOT due to OMI (normal variant, pericarditis)
4. If a patient presents with symptoms of ACS, has an elevated troponin, and has persistent symptoms in spite of medical therapy [antiplatelet, antithrombotic, and anti-ischemic (nitro)], then cath lab activation is indicated regardless of ECG findings.
5. Compare with an old ECG.
6. Record serial ECGs.
Time zero
 |
| What do you think? |
There is inferior ST elevation. Is it normal variant? Is it ischemic (OMI)? [Pericarditis? (NOT!)]
There is one finding that argues against inferior OMI (There is absence of reciprocal ST depression in aVL; STD aVL is extremely sensitive for inferior OMI; Reference: Bischof and Smith).
However, there is also straightening of the inferior ST segments, and a straight ST segment in aVF; this is extremely rare in normal variant STE).
_______
There is also terminal QRS distortion in II, III, aVF [absence of S-wave and J-wave (notch)]. The significance of this in inferior leads is unknown, but I suspect it is a marker for inferior OMI vs. normal variant.
Terminal QRS distortion is definitely significant for anterior OMI in V2 and V3:
An intoxicated, agitated, 20-something with chest pain
______Here is an ECG from one month ago:
 |
| There is a definite change in the inferior leads, with new ST elevation. Previously, all inferior leads had appropriate upward concavity. |
The patient was given aspirin, heparin, and IV nitroglycerine.
Another ECG was recorded at 35 minutes:
 |
| It is hard to discern a difference |
At this point, the first troponin I returned at 0.55 ng/mL (significantly elevated)
A D dimer was also elevated.
Another ECG was recorded at 58 minutes:
 |
| Again, no big difference. |
There was concern for aortic dissection, so a CT was done and was negative.
The cath lab was activated:
Result: Thrombotic 95% stenosis at the ostium of a small LPL2 with 70% stenosis at the LPL2/LPDA bifurcation in the distal/AV groove Cx Tubular 70% stenosis in the mid-circumflex. (In other words, inferior MI with some posterior involvement). It was stented.
For coronary anatomy, see here: https://www.pcipedia.org/wiki/Coronary_anatomy
For coronary anatomy, see here: https://www.pcipedia.org/wiki/Coronary_anatomy
This is the post intervention ECG:
 |
| All ST Elevation is gone (more proof that it was all a result of ischemia) |
Normal estimated left ventricular ejection fraction - 55%.
Regional wall motion abnormality-mid and basal inferior .
Troponin I peaked at 12.1 ng/mL.
Learning Points:
1. Any inferior ST elevation may be acute OMI, but there are subtle differences between OMI on the one hand, and normal variant on the other.
2. 99% of inferior OMI are either obvious or have some amount of ST depression in aVL. But 1% may be/have neither!
3. In this case, one might say it is "obvious" MI because of a straight ST segment in aVF. A straight ST segment virtually never happens in inferior ST elevation that is NOT due to OMI (normal variant, pericarditis)
4. If a patient presents with symptoms of ACS, has an elevated troponin, and has persistent symptoms in spite of medical therapy [antiplatelet, antithrombotic, and anti-ischemic (nitro)], then cath lab activation is indicated regardless of ECG findings.
5. Compare with an old ECG.
6. Record serial ECGs.
===================================
Comment by KEN GRAUER, MD (6/28/2019):
===================================
I like this case because it provides an excellent example of how to use comparison tracings in a patient with a prior history of coronary disease.
- For clarity — I’ve put the first 2 ECGs shown in this case together in Figure-1. To highlight KEY findings — I’ve enlarged one complex in leads II, III, aVF and aVL, that I’ve placed to the right of each of the 12-leads.
 |
| Figure-1: The first 2 ECGs shown in this case — with enlargement of leads II, III, aVF and aVL to the right of each tracing (See text). |
The CASE: The patient is a 60-something who presented to the ED with new-onset chest pain. The patient had a prior history of MI + stents.
- KEY Points: This patient has known coronary disease. Therefore: i) The initial ECG may show signs of prior injury; ii) ECG evidence of new OMI may be subtle; it may be difficult to distinguish “new” from “old” ECG findings from the initial ECG alone (ie, from ECG #1 alone in Figure-1); and, iii) Finding a prior ECG on this patient may provide invaluable assistance!
QUESTION: — regarding ECG #1: Before you looked at the prior ECG in this case (which is ECG #2 in Figure-1) — YOU should have seen 3 abnormal findings in the chest leads of ECG #1! — Did you see these 3 abnormal findings ??? —
- HINT: It would have been EASY to overlook these 3 findings if you were not Systematic in your interpretation ...
My THOUGHTS on ECG #1 — The rhythm is fairly regular, at a rate between 55-60/minute. The QRS is narrow. This is sinus bradycardia.
- All intervals (PR, QRS duration, QTc) are normal.
- The frontal plane axis is normal (about +65 degrees).
- There is no chamber enlargement.
Regarding Q-R-S-T Changes:
- There are Q waves in multiple leads, including leads I, II, III, aVL, aVF; and in leads V3-thru-V6. Most of these Q waves are small and narrow. Many are unlikely to be clinically significant. That said — although tiny, the Q in aVL of ECG #1 could reflect lateral MI of uncertain age given how small the QRS is in this lead (Note in the Blow-Up view that the initial deflection in lead aVL of ECG #1 is negative = a Q wave).
- While the Q waves in leads V4, V5 and V6 are narrow — they are a little deeper-than-usual for normal septal q waves. In this patient with documented coronary disease — these q waves could reflect prior lateral infarction (especially in view of the Q in lead aVL).
- Regarding R Wave Progression —Transition is early! In fact — R = S in lead V1, and this is not a “normal” finding! Because LV (left ventricular) forces predominate in a normal ECG — there is usually no more than a small initial r wave in lead V1, which is normally associated with a fairly deep S wave in lead V1 (this deep negative deflection in right-sided lead V1 results from the normal predominance of LV forces).
- NOTE: Computer interpretations almost always miss detection of a Tall R Wave in Lead V1. Many (if not most) clinicians also often overlook this important finding if they are not systematic in their approach. This is precisely the reason why I add an “R” to my memory aid of looking for “Q-R-S-T Changes” — because it is otherwise all-too-easy to forget about routinely looking to see if R wave progression is appropriate.
- PEARL: Recognition of a Tall R Wave in Lead V1 should prompt quick recall of a list of the 6 Common Causes — one of which is posterior MI. This is highly relevant to this case! (CLICK HERE — for discussion on how to distinguish between these 6 entities).
- For review of “My Take” on the Systematic Approach to ECG Interpretation that I favor — CLICK HERE —
Returning to this case for the last 2 parameters in my Q-R-S-T assessment of ECG #1 = ST-T Wave Abnormalities:
- We’ve already noted small-but-present-in-all-3-inferior-lead Q waves. The Blow-Up view to the right of 12-lead for ECG #1 shows the features already highlighted above by Dr. Smith = inferior lead ST elevation + straightening of the ST segment upstroke in lead aVF + terminal QRS distortion (ie, lack of an S wave and J wave) in each of the 3 inferior leads. More than this, the ST-T waves in each of these inferior leads just “look” acute (with T waves taller-and-fatter-than-they-should-be).
- The T wave in lead aVL of ECG #1 is not normal. Instead, the entire ST-T wave in lead aVL is flat — and it shouldn’t be.
- In the chest leads — T waves in leads V2-thru-V5 (if not also in V6) appear taller-and-more-peaked-than-they-should-be. While I doubted hyperkalemia as the cause — I’d check serum K+ to be sure. More likely, these T waves probably reflect ischemia of uncertain age.
My IMPRESSION of ECG #1: In this patient with a history of documented coronary disease + new-onset chest pain — one has to assume new inferior OMI until proven otherwise.
- ANSWER to the above QUESION: The 3 abnormal ECG findings in the chest leads of ECG #1 that you should have noted before you looked at ECG #2 are: i) The Tall R Wave in lead V1; ii) The Q waves that begin as early as lead V3, and which are a bit deeper-than-is-usually-seen in leads V4, V5 and V6; and, iii) Chest lead T waves that are taller-and-more-peaked-than-usual. In view of this patient’s history — the combination of these ECG findings suggests possible infero-postero-lateral MI of uncertain age (probably new-upon-old injury). Of note — cath findings on this patient are consistent with my impression of these 3 abnormal findings.
My THOUGHTS on ECG #2 — ECG #2 was done 1 month earlier on this patient.
- NOTE: We are not told about what was going on clinically 1 month earlier at the time ECG #2 was recorded (ie, we don't know if the patient was admitted for their initial event during that earlier admission). That said — what we can say, is that there has been NO change in chest lead appearance between the time that ECG #1 and ECG #2 were done.
- I would have loved to see an ECG on this patient prior to development of coronary disease. I bet that the R wave would not be comparable to S wave size in lead V1 — and, I bet chest lead T waves were not so peaked. I’d also be curious to see if there were Q waves of similar size in leads V3-thru-V6 on a prior tracing.
What is different between ECG #1 and ECG #2 — is easily seen in the magnified leads of the Blow-Up magnifications in Figure-1 to the right of each 12-lead.
- As emphasized by Dr. Smith — 1 month earlier, there was no ST elevation in any of the inferior leads. This confirms that there is a new inferior OMI in ECG #1!
- Note that 1 month earlier — the ST-T wave in lead aVL looks very different! Thus, in the Blow-Up of ECG #2 — lead aVL showed slight-but-real ST elevation with an upright T wave. This tells us that the flat ST-T wave in lead aVL of ECG #1 actually was reflective of acute reciprocal change (ie, in response to new inferior lead ST elevation — the ST segment and T wave in lead aVL of ECG #1 was acutely lowered compared to what it was 1 month earlier).
- Note also that there is now no doubt from the Blow-Up of ECG #2 that an abnormal Q wave was already present in the earlier tracing ( = ECG #2) in lead aVL — most probably reflecting a prior lateral infarction.
Additional Learning Points:
- Sometimes acute reciprocal changes in lead aVL may be masked by prior abnormalities in an earlier tracing. The flat ST-T wave in lead aVL of ECG #1 actually did represent acute reciprocal change — since a month earlier the T wave in this lead was upright, and the ST segment was slightly elevated.
- It’s easy to miss abnormal ECG findings if you fail to routinely use a Systematic Approach. Thus, in ECG #1 — the Tall R in lead V1 + the more-peaked-than-expected chest lead T waves + all of those lateral lead Q waves were probably all findings reflective of this patient’s prior coronary injury and coronary anatomy (with disease in the posterior and circumflex circulation). The importance of not overlooking these findings — is that we would not be able to exclude the possibility that these were acute changes if all we had to look at was ECG #1. It was only after locating the tracing from 1 month earlier that we were able determine that none of the chest lead findings in ECG #1 were acute.