What do you think of these 2 ECGs in patients with chest pain? How to approach these?
ECG 1 (sent to my by Sam Ghali @EM_resus)
ECG 2
ECG 1
This was sent to me with no clinical information and the question "what do you think?"
My answer was: "sinus rhythm with right atrial enlargement, probable right ventricular hypertrophy, and old inferior MI with inferior LV aneurysm." The T-wave inversion in I and aVL is reciprocal to the Old inferior aneurysm.
After I sent my answer, I received this history:
66 yo man presented with chest pain
ECG 2
I was reading ECGs on the system and came across ECG 2 and said out loud: "This is a fake." A colleague sitting next to me asked "why?", and I answered that there is a "saddleback" in lead III and well-formed Q-wave. Saddleback ST elevation is rarely due to OMI.
However, on very few occasions Saddleback STE actually is due to OMI.
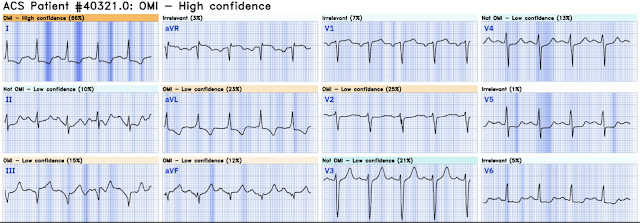
The Queen of Hearts had stated "Not OMI with low confidence"
There was a previous ECG available:
This Queen interpretation led to a false positive cath lab activation.
A Patient with Vertigo
An Akinetic wall can have the same "LV aneurysm" Morphology as a Dyskinetic wall ("diastolic dyskinesis" is the echo definition of aneurysm.)
The cath lab was activated and there was no acute OMI. False Positive.
Discussion:
These are very complex cases in which there could be OMI or there could be old MI. These are the kind of cases in which you want to consult your friendly cardiologist and have a discussion. But that is only if your cardiologists accept the idea of OMI (Acute Coronary Occlusion in the Absence of ST Elevation criteria). To make such a consultation, there must be mutual trust that the consultant will not dismiss your concerns or say "Nah, couldn't be."
It can take years to build such trust.
MY Comment, by KEN GRAUER, MD (7/30/2024):
- For clarity and ease of comparison in Figure-1 — I've labeled and put together the initial 2 ECGs in today's case.
- There is significant baseline artifact. This is relevant to our interpretation given the difficulty it poses for assessment of ST-T wave changes in multiple leads.
- That said — the rhythm is clearly sinus with a normal PR interval.
- QRS morphology is not normal. That said — the QRS is really not wide (ie, not more than 0.10 second). Given the all upright QRS complex in lead V1, with narrow but definite terminal S waves in lateral leads I and V6 — this QRS morphology is consistent with IRBBB (Incomplete Right Bundle Branch Block).
- The QTc is prolonged (I measure the QT at ~0.44 second — which corrected for the rate of ~80/minute, comes out to a QTc ~0.49 second).
- There is marked LAD (Left Axis Deviation) — with entirely negative QRS complexes in each of the inferior leads. This is consistent with LAHB (Left Anterior HemiBlock).
- There is RAA (Right Atrial Abnormality) — as determined by the presence of tall, peaked and pointed P waves in the inferior leads (ie, P waves ≥2.5 mm in amplitude).
- There may be RVH (Right Ventricular Hypertrophy) — which always needs to be considered if there is true right atrial enlargement. Because of the artifiact — we can not tell if QRS morphology in lead V1 is triphasic (rsR') or represents a qR pattern, which could be consistent with pulmonary hypertension (for more on RAA, RVH — See My Comment in the February 12, 2023 post).
- There may be LVH by Peguero criteria (See My Comment in the June 20, 2020 post) — as suggested by the very deep S waves in leads V3 and V4 (with the PURPLE arrow in lead V3 showing that S wave amplitude is cut off in this lead).
- More than inferior Q waves — there is marked fragmentation on each downslope of the S wave in the inferior leads (RED arrows in these leads). It is because of this marked fragmentation that the “attempt” to form a positive deflection in each inferior lead never makes it back to the baseline before being overtaken by resumption of S wave negativity. In my experience — this fragmented QRS shape in any one (let alone all 3) of the inferior leads strongly suggests inferior infarction at some point in time.
- Regarding R wave progression — I interpreted the seemingly multi-phasic upright complex in lead V1 as the result of IRBBB rather than RVH because: i) There is marked LAD with no more than modest depth of the S wave in lead I; and, ii) I thought the overall ECG picture more suggestive of coronary disease rather than RVH. Yet predominant positivity never occurs in the lateral chest leads — and I could not rule out the possibility of RVH on this ECG alone.
- The shape of the S-T segments in the inferior leads is coved, of relatively long duration, and shows slight ST elevation. This shape forms a “picture to remember” — that does not look acute. That this inferior lead ST-T wave appearance is unlikely to be acute — is further supported by a lack of reciprocal ST depression in high-lateral leads I and aVL. Instead (as per Dr. Smith) — this “picture” strongly suggests inferior wall aneurysm, especially given the inferior lead S wave fragmentation marker of prior inferior MI described above.
- Finally — there is ST segment straightening and depression beginning in lead V3 beyond that expected for simple IRBBB (BLUE arrows in the chest leads).
- I suspected prior inferior MI with IRBBB/LAHB — and now with inferior wall aneurysm. There is ST depression in leads V3-thru-V5 that I thought likely to reflect multi-vessel disease — but with need to explain the reason for RAA, probable LVH, and possible RVH. But – not an OMI.
- As per Dr. Smith — this patient turned out to have Troponin elevation due to Type-2 MI (clean coronaries on cath). Instead — his clinical presentation was dominated by acute renal failure with severe acidosis. We are left with more questions than answers (ie, How severe is his underlying coronary disease? Any RVH or pulmonary hypertension?) — but this is not the ECG of acute coronary conclusion.
- Personal NOTE: I have been fooled more than once by chest pain in the setting of severe underlying disease (ie, acidosis, sepsis). The KEY is to recognize that ECG #1 is unlikely to represent an acute OMI — with clinical priority to treat underlying conditions, and to then reassess symptoms and repeat ECGs as needed.
-USE.png) |
| Figure-1: I've labeled the initial 2 ECGs in today's case. |
- The rhythm is sinus — with normal intervals (PR-QRS-QTc). There is LAD (negative QRS in lead aVF) — but an axis not leftward enough to qualify as LAHB (predominant positivity in lead II).
- There is no chamber enlargement.
- There are very large and wide Q waves in leads III and aVF — with a small-but-present Q wave in lead II (RED arrows in these leads). This patient has had inferior infarction at some point in time.
- R wave progression shows slight delay in transition (the R wave only becomes taller than the S wave is deep between lead V4-to-V5).
- S-T elevation is seen in each of the inferior leads, followed by a prominent upright T wave. That said — the shape of the elevated inferior lead ST segments manifests an upward concavity (ie, "smiley" configuration). As per Dr. Smith — this shape is less likely to represent an acute cardiac event.
- Although both high-lateral leads ( = leads I and aVL) manifest ST depression — the precise mirror-image opposite ST-T wave picture from lead III — is seen in lead aVL (within the BLUE rectangle, in which I merely inverted one QRST complex from lead III). This to me suggested a similar acuity (or lack thereof) for both lead aVL and the inferior leads.
- There is slight, nonspecific ST-T wave flattening in leads V1,V2 and V6.
- The deep, wide Q waves in leads III and aVF (with small-but-present Q in lead II) — strongly suggest prior infarction. This patient almost certainly does have underlying coronary disease. Clinically, if I was managing this patient — more information would clearly be needed (ie, specifics of the history; repeat ECG; troponins; comparison with prior tracings, etc.). But as a single ECG without the benefit of more information — the shape of these inferior lead ST segments — and the lack in the chest leads of any suggestion of associated acute posterior involvement — suggest this is not the result of acute coronary conclusion.
- As per Dr. Smith — review of this patient's chart told the story. Not surprisingly — the patient had very severe underlying coronary disease — but no acute OMI.







-USE%20copy.png)

-USE.png)
-USE.png)