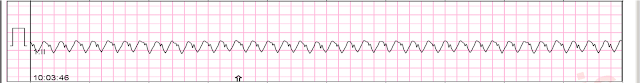
An older patient with no previous medical history arrived at triage complaining of SOB. Her heart rate was very fast, so we obtained an ECG immediately:
ECG:
There is a regular wide complex tachycardia. The QRS morphology is RBBB with LAFB (tiny r-waves in inferior leads followed by deep S-waves; tiny q-wave in aVL followed by large R-wave; Left axis deviation). There appears to be a sawtooth pattern in lead II. There is a fully upright "P" wave about midway between each QRS in V1.
A fully upright P-wave is typical atrial activity of atrial flutter as seen in V1.
See these example cases of upright P-waves:
Case Continued
Thus, I was all but certain that this was atrial flutter.
I brought the patient to the critical care area and told the providers I thought it was atrial flutter with 2:1 AV conduction, but there is an outside chance that it is VT. If they want to confirm, they could give adenosine and "uncover" the flutter waves.
Remember: Adenosine is safe in Regular Wide Complex Tachycardia. If it is VT, there will be no effect. If it is antidromic AVNRT or AVRT (WPW, accessory pathway), it will convert. If it is flutter, it will reveal the underlying flutter waves.
[Adenosine is only unsafe in atrial fibrillation with WPW, which presents with a very rapid rate, polymorphic QRS, and some very short RR intervals]
Bedside echo showed poor LV fct. BP was 100 systolic.
They chose to give adenosine, and this is what happened:
Adenosine to verify flutter: flutter waves made obvious
Very Fast Very Wide Complex Tachycardia
Ideally, one would cardiovert.
Several hours later, this was the effect:
NT pro-BNP elevated to 7000
Furosemide was also given.
A formal ultrasound later showed reasonably good LV function, and so he later received carvedilol and diltiazem, Unfortunately, those led to hypotension at 80/40 with a HR 40.
Eventually the patient stabilized on Carvedilol 25 mg bid and Diltiazem 60 mg po q 6 hours
The patient did not want a TEE (transesophageal echo to rule out atrial thrombus), so anticoagulation was started with a plan for outpatient cardioversion in 4 weeks
What happens when you give adenosine to a patient with this rhythm?
MY Comment, by KEN GRAUER, MD (7/5/2024):
- As we often emphasize (See My Comment in the May 5, 2020 post of Dr. Smith's ECG Blog) — Statistically (ie, even before we look at the ECG itself) — at least 80% of all regular WCT rhythms without clear sign of P waves will turn out to be VT (Ventricular Tachycardia). This is especially true in an older adult, as is the patient in today's case. As a result — we need to always assume VT until proven otherwise.
- That said — As per Dr. Smith, there are times when morphologic clues suggest that a WCT rhythm is supraventricular, either with preexisting BBB (Bundle Branch Block) — or, with aberrant conduction.
- As per Dr. Smith — Today's initial ECG shows a regular WCT rhythm at just under 150/minute, without sinus P waves (ie, there is no clearly upright P wave in lead II with a reasonable chance to conduct).
- QRS morphology is consistent with RBBB/LAHB conduction (ie, upright QRS in V1 with wide terminal S wave in V6 — and predominant negativity in the inferior leads). That said — the lack of a terminal S wave in lateral limb leads I and aVL is atypical for true RBBB conduction. As a result — We can not rule out VT on the basis of this single ECG.
- The BEST way not to miss the diagnosis of AFlutter — is to always consider AFlutter whenever you have a regular SVT (SupraVentricular Tachycardia) at a rate close to 150/minute.
- PEARL #2: Using calipers facilitates recognition. What makes the rhythm in ECG #1 so challenging to diagnose — is that atrial activity is partially hidden within the QRS and ST-T wave. This is where calipers help. Simply set your calipers to precisely half the R-R interval. Then see if you can "walk out" 2:1 atrial activity in any of the 12 leads.
- KEY Point: My "Go-To" leads when looking for subtle atrial activity are the inferior leads (II,III,aVF) — lead aVR — and lead V1, as these are the leads most like to reveal "hidden clues" when atrial activity is not readily apparent.
- Normally, this beginning portion of the ST segment should be smooth. The magnified view of lead II in Figure-1 makes it easier to appreciate the perfect 2:1 regularity of these small-amplitude positive deflections that occur at a rate of ~300/minute. The only thing that does this is AFlutter!
- To Emphasize: This 2:1 atrial activity that I highlight in Figure-1 is subtle. It will not be seen unless you specifically look for it. And, the reasons I immediately looked in my 5 "Go-To" leads for subtle signs of extra atrial activity are: i) That QRS morphology in ECG #1 is consistent with RBBB/LAHB conduction, therefore potentially consistent with a supraventricular etiology; and, ii) That the rate of today's regular tachycardia is close to 150/minute (ie, Therefore by PEARL #1, the need to consider AFlutter as the potential etiology).
-USE.png) |
| Figure-1: I've labeled atrial activity in today's ECGs. |
- PEARL #3: Odd conduction ratios with AFlutter are uncommon (if not rare!). As emphasized above — by far, the most common conduction ratio of untreated AFlutter is 2:1, which typically results in a ventricular rate of ~150/minute (usual range ~140-160/minute).
- The next most common conduction ratio with AFlutter is 4:1 — which is what we see in Figure-1.
- 1:1 and 3:1 conduction ratios are seen far less often. The clinical relevance of appreciating these conduction ratios — is that a regular tachycardia of ~110/minute is far less likely to represent untreated AFlutter — because 110 X 2 = 220/minute, which is considerably slower than the usual ventricular rate response for untreated AFlutter (ie, The atrial rate of flutter may be less if the patient is being treated with an antiarrhythmic agent).
- 1:1 AV conduction with AFlutter is rare. About the only times I have seen this is with WPW (ie, accelerated conduction over an accessory pathway) — or, in a patient with AFlutter who is treated with an antiarrhythmic such as Flecainide, but without an AV nodal blocking agent to control the ventricular response.
- Having trained in the 1970s — I had lots of experience using oral and IV Digoxin. At the time, it seemed that virtually all cardiac patients with chronic AFib or heart failure were on this medication. The drug works — but caution is needed in use because of the risk of Dig toxicity.
- In recent decades — Digoxin has been used much less often. As a result — current generations of physicians have far less experience using this medication. I believe ( = My opinion) this reduced use of Digoxin is appropriate for 2 reasons: i) In most circumstances — other more effective agents are available; and, ii) It is because recent generations of physicians have less experience using Digoxin — that the risk of developing Dig toxicity in their hands is increased. The drug is effective — but there is an "art" to optimal use.
- The above said — Dr. Smith's skillful use of IV Digoxin loading in today's case illustrates successful use in this special situation.
- PEARL #4: While onset of action following oral ingestion of Digoxin is between 30 minutes to 2 hours — the onset of action following IV administration may begin within 15-to-30 minutes (Ferrari et al — Current Cardiol Rev, 16(2): 141-146, 2020 — and — London Health Sciences Centre, 2018). IV Digoxin may begin to slow the ventricular response of AFib or AFlutter sooner than many clinicians realize.





No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.