This middle-aged man with no cardiac history but with significant history of methamphetamin and alcohol use presented with chest pain and SOB, worsening over days, with orthopnea.
BP:143/99, Pulse 109, Temp 37.2 °C (99 °F), Resp (!) 32, SpO2 95%
On exam, he was tachypneic and had bibasilar crackles.
Here was his ED ECG:
NT-ProBNP was 8316 (0-900 pg/mL).
"NT-proBNP values less than 300 pg/ml have a 99% negative predictive value for excluding congestive heart failure. A cutoff of 1200 pg/ml for patients with a normal eGFR is very specific for heart failure. A diagnostic NT-proBNP cutoff of 900 pg/mL has been suggested in adults 50-75 years of age in absence of renal failure."
A bedside POC cardiac ultrasound was done:
Findings: Decreased left ventricular systolic function.
The patient was given furosemide and admitted to the hospital.
Later, he underwent a formal echocardiogram:
Later, he was noted to have a very rapid heart rate. An ECG was recorded:
The tachycardia spontaneously resolved. The post tach ECG is similar to the first one:
The tachycardia recurred and resolved.
This was recorded the next day:
See Ken Grauer's Analysis Below. Ken has a very detailed analysis and shows that, without an EP study, we cannot know whether this is PAT or "Fast-Slow form of AVNRT". He favors the latter.
In any case, what would you do if you saw this?
Try adenosine. It works for many forms of PAT and also of course for AVNRT or AVRT.
Patient course
The patient was started on beta blockers and schedule for an electrophysiologic study.
Unfortunately, that EP study has not yet been done.
The new onset cardiomyopathy was thought to be due to both drug/alcohol use and to Tachycardia-Induced Cardiomyopathy.
Here is one full text article on the topic from Clinical Cardiology 2008: Diagnostic Approach and Treatment Strategy in Tachycardia-induced Cardiomyopathy
Atrial Tachycardia (AT): another SVT in the ED
Rapid dysrhythmia from non-sinus focus above AV node.
Atrial Flutter is a type of atrial tachycardia which is "Macro-reentrant," meaning that the re-entry loop is quite large, encircling much of the atrium, and you can actually see that loop on the surface 12-lead as flutter waves.
The other atrial flutter types are:
1. Micro-reentrant (Paroxysmal Atrial Tachycardia -- PAT), which produce an atrial wave which may resemble a P-wave, but be larger or inverted of different morphology.
2. Automatic (the sinus node is also an automatic rhythm). Automatic rhythms cannot be broken adenosine. They rely on phase 0 depolarization until threshold is met.
3. Triggered
General Statements about AT
Etiology
Summary of Adenosine in Atrial Tachycardia
BP:143/99, Pulse 109, Temp 37.2 °C (99 °F), Resp (!) 32, SpO2 95%
On exam, he was tachypneic and had bibasilar crackles.
Here was his ED ECG:
NT-ProBNP was 8316 (0-900 pg/mL).
"NT-proBNP values less than 300 pg/ml have a 99% negative predictive value for excluding congestive heart failure. A cutoff of 1200 pg/ml for patients with a normal eGFR is very specific for heart failure. A diagnostic NT-proBNP cutoff of 900 pg/mL has been suggested in adults 50-75 years of age in absence of renal failure."
A bedside POC cardiac ultrasound was done:
Findings: Decreased left ventricular systolic function.
The patient was given furosemide and admitted to the hospital.
Later, he underwent a formal echocardiogram:
Very severe left ventricular enlargement (LVED diameter 7.4 cm).
Severely decreased left ventricular systolic function with an estimated EF of 20-25%.
No left ventricular wall motion abnormality identified.
Severe right ventricular enlargement and mildly decreased right ventricular systolic function.
Mild to moderate mitral regurgitation.
Biatrial enlargement, severe.
The absence of any wall motion abnormality makes ischemic cardiomyopathy very unlikely. Therefore, no angiogram was done.
Later, he was noted to have a very rapid heart rate. An ECG was recorded:
The tachycardia spontaneously resolved. The post tach ECG is similar to the first one:
 |
| Sinus rhythm |
The tachycardia recurred and resolved.
This was recorded the next day:
See Ken Grauer's Analysis Below. Ken has a very detailed analysis and shows that, without an EP study, we cannot know whether this is PAT or "Fast-Slow form of AVNRT". He favors the latter.
In any case, what would you do if you saw this?
Try adenosine. It works for many forms of PAT and also of course for AVNRT or AVRT.
Patient course
The patient was started on beta blockers and schedule for an electrophysiologic study.
Unfortunately, that EP study has not yet been done.
The new onset cardiomyopathy was thought to be due to both drug/alcohol use and to Tachycardia-Induced Cardiomyopathy.
Here is one full text article on the topic from Clinical Cardiology 2008: Diagnostic Approach and Treatment Strategy in Tachycardia-induced Cardiomyopathy
Atrial Tachycardia (AT): another SVT in the ED
Rapid dysrhythmia from non-sinus focus above AV node.
Atrial Flutter is a type of atrial tachycardia which is "Macro-reentrant," meaning that the re-entry loop is quite large, encircling much of the atrium, and you can actually see that loop on the surface 12-lead as flutter waves.
The other atrial flutter types are:
1. Micro-reentrant (Paroxysmal Atrial Tachycardia -- PAT), which produce an atrial wave which may resemble a P-wave, but be larger or inverted of different morphology.
2. Automatic (the sinus node is also an automatic rhythm). Automatic rhythms cannot be broken adenosine. They rely on phase 0 depolarization until threshold is met.
3. Triggered
General Statements about AT
•Regular, Rate 150-250
•P’s before QRS (different morphology),
Constant P’-
R interval
•Sinus node re-entry tachycardia
•Automatic (NPAT), due to adrenergic stim of normal atrial
tissue
•Gradual in onset
•Transient suppression by adenosine
•Re-entrant (paroxysmal, PSVT, PAT)
•Abrupt onset
•Intra-atrial re-entry
•Abnormal atrium, esp. after atrial
surgery
•Not stopped by adenosine (0/13 pts, incl. 8 with flutter)
•Electricity works
•Sinus node re-entry--(within the sinus node!) Adenosine works
•Triggered (paroxysmal)
•Cardiomyopathy, on digoxin, usually some AV block
•Prolonged and difficult to treat
Etiology
Lytes, acid-base, drug tox, fever, hypoxia,
thyroid, cardiac surgery
•Digitalis
toxicitiy
•Correct hypokalemia, Digibind
Management
Correct
underlying disturbance
•Beta
blocker or Ca channel blocker
•Mg
(2-4 g IV)
•Adenosine
occasionally terminates
•Sinus node re-entry or triggered activity
•Electrical
treatment rarely needed
•50-100 J if unstable
•Overdrive
transvenous atrial pacing
Adenosine:
Atrial tachycardia
PAT
efficacy: depends on which etiology
•Automatic (transient slowing)
•Re-entrant in non-sinus atrial tissue (no effect, as in
flutter)
•Re-entrant in sinus node (terminates)
•Triggered – it works
•Atrial
myocytes
•Shortens atrial action potential duration
•Does not hyperpolarize
•No effect on intra-atrial re-entry
•Sinus
node
•Hyperpolarization
•Stops sinus node re-entry PAT
•Temporarily inhibits sinus rhythm
•Shortens atrial action potential duration
•Anti-adrenergic--Inhibition of cAMP--Stops cAMP-triggered
activity
•Just try it
--Adenosine
aborts some paroxysmal PAT, but not all.
--You
may not know that the PSVT is PAT
--If
adenosine doesn’t work for SVT
It may be atrial tachycardia
--If
adenosine does work for PAT
You’ll
think you treated AVNRT
--If
you do diagnose PAT
Adenosine is worth a try
===================================
MY Comment by KEN GRAUER, MD (3/6/2020):
===================================
Interesting case of this patient with severe, dilated cardiomyopathy + alcohol abuse, who presented to the ED with acute, decompensated heart failure + an episode of SVT ( = SupraVentricular Tachycardia). I focus My Comment on determination of the etiology of this patient’s tachyarrhythmia — and compare it to other SVT rhythms previously published in Dr. Smith’s ECG Blog.
- Dr. Smith shows 4 tracings on the patient in Today's Case (shown above) — the 2nd and 4th of these tracings show the same tachyarrhythmia. Since the 4th tracing (obtained on this patient the following day) captured a PVC near the end of the recording — I chose to use this 4th tracing in my discussion (to illustrate how the occurrence of a PVC during an SVT rhythm may help in diagnosis).
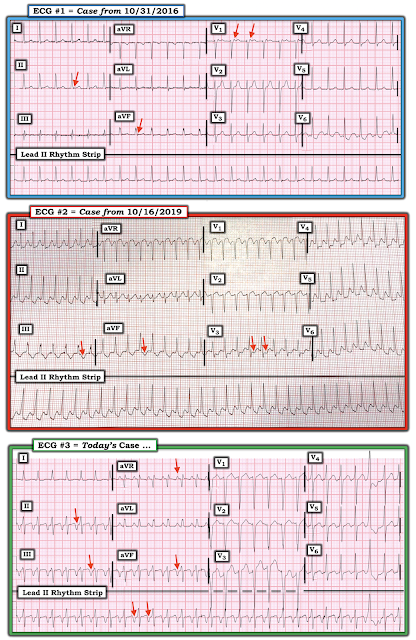 |
| Figure-1: Three cases of a regular SVT without clear sign of sinus P waves (See text). |
NOTE: I begin with Figure-1 — in which I show 3 examples of Regular SVT rhythms, in which sinus P waves (ie, upright P waves in lead II) are not seen:
- ECG #1 in Figure-1 is from the October 31, 2016 post on Dr. Smith’s Blog.
- ECG #2 in Figure-1 is from the October 16, 2019 post on Dr. Smith’s Blog.
- ECG #3 in Figure-1 is the 4th tracing shown above from Today’s Case.
For interest — I have added some RED arrows to each of the 3 tracings in Figure-1. Again — each of these tracings show a Regular SVT rhythm, in which sinus P waves (ie, upright P waves in lead II) are not seen.
QUESTIONS:
- Regarding these RED arrows in Figure-1 — What do each of these 3 tracings have in common?
- What is different about these RED arrows in these 3 tracings?
- What are the diagnostic possibilities (and probabilities) in each case?
- Clinically — WHY does this matter?
General Thoughts on the ECG Diagnosis of SVTs: The term, “SVT” ( = SupraVentricular Tachycardia) is often misunderstood. This is a “generic” term. By this I mean — that it includes all arrhythmias in which the rate is “Tachycardic” (ie, ≥100/minute in an adult) — and, in which the rhythm is “SupraVentricular” (ie, originating at or above the AV node).
- Terminology: Many providers (including even experienced providers) — use the term “SVT” when speaking about a reentry supraventricular tachycardia (ie, AVNRT or AVRT). But since the term “SVT” really includes all arrhythmias with a rate ≥100/minute that originate at or above the AV node — this term also includes sinus tachycardia + junctional tachycardia + atrial fibrillation (AFib), atrial flutter (AFlutter) and MAT (Multifocal Atrial Tachycardia) IF the average ventricular response is fast enough + automatic atrial tachycardia (ATach) + a number of selected other less common SVT rhythms such as sinoatrial node reentry tachycardia.
- Most SVT rhythms manifest a narrow QRS complex. That said — an SVT rhythm may have a wide QRS if there is either preexisting bundle branch block or aberrant conduction due to the rapid rate.
- Practically Speaking — the principal differential diagnosis of a Regular SVT rhythm, in which sinus P waves (ie, a definite upright P wave in lead II) are not evident includes: i) Sinus Tachycardia (IF there is a possibility that sinus P waves might be hiding within the preceding ST-T wave); ii) A Reentry SVT (either AVNRT if the reentry circuit is contained within the AV node — or AVRT if an AP [Accessory Pathway] located outside the AV node is involved); iii) Atrial Tachycardia; or iv) Atrial Flutter with 2:1 AV conduction.
- Heart Rate Can Help! I review my Systematic Approach to Rhythm Interpretation in detail in My Comment to the October 16, 2019 post on Dr. Smith’s ECG Blog. In brief — i) IF the heart rate in an adult is ≥170/minute — then both Sinus Tachycardia and AFlutter become less likely (ie, not impossible! — but less likely); — BUT — ii) IF the heart rate of a regular SVT rhythm in an adult is close to ~150/minute (ie, ~140-160/minute) — then any of the above 4 entities have to be considered in the differential diagnosis!
- Detection of Atrial Activity! — I have previously reviewed how using calipers can facilitate detection of 2:1 AV conduction that can be diagnostic of AFlutter (See My Comment in the November 12, 2019 post of Dr. Smith’s ECG Blog). As we will see below — detection of retrograde atrial activity can be diagnostic of a reentry SVT rhythm.
- PEARL #1 — Look for a “Break” (or subtle Change) in the Rhythm! — Even a slight pause in the rhythm, may be all that is needed to reveal underlying atrial activity that had been hidden by the tachycardia. For example — WHAT happens toward the end of the tracing in ECG #3?
- PEARL #2 — Look for the “Onset” (and/or Termination) of the Rhythm! — The KEY clue to the etiology of an SVT often lies with capturing either the beginning and/or the end of the SVT. ATach often begins gradually, with progressive acceleration of the ectopic focus (ie, “warm-up” phenomenon). Then, there may be gradual slowing (ie, “cool-down”) of the rhythm as it ends. In contrast — SVT reentry rhythms often start with 1 or more PACs that block conduction down one of the AV nodal pathways, setting up the reentry circuit as the impulse starts down the other pathway. The onset of a reentry SVT is often abrupt (ie, accounting for the previous term used to designate this rhythm = PSVT = Paroxysmal SVT). The termination of reentry is usually quick — though this may occur over several beats.
- The “Good News” Regarding SVT Treatment — It is true that determining the specific rhythm diagnosis facilitates management. This is especially important IF the rhythm turns out to be sinus tachycardia — in which case, finding and treating the underlying cause of sinus tach is KEY for optimal management. It is also true that various antiarrhythmic agents may be used somewhat differently, depending on the specific rhythm diagnosis. However, for practical purposes — initial treatment measures in the field or in the ED are quite similar for virtually all of the above rhythms = Consider vagal maneuvers and/or use of an AV nodal blocking agent (ie, Verapamil/Diltiazem, a ß-Blocker, Adenosine).
What About the RED Arrows in Figure-1? — Each of the 3 tracings show in Figure-1 show a Regular SVT rhythm, in which sinus P waves (ie, upright P waves in lead II) are not clearly seen.
- ECG #1 — shows a regular SVT at just under 150/minute. The upright deflection near the midpoint in the R-R interval in lead II is almost certainly just a T wave. Against there being a sinus P wave hidden within this T wave — is the fact that this would make the PR interval long (ie, ~0.26 second) — and if anything, the PR interval shortens when there is tachycardia. Although the rate of ~150/minute should make you think about the possibility of AFlutter — other than lead V6, none of the other 11 leads even remotely suggest 2:1 AV conduction. The RED arrows in ECG #1 — suggest retrograde atrial conduction with a very short RP’ interval (RP' << PR) that notches the terminal portion of the QRS complex (with a positive deflection in lead V1 — and — with suggestion of a negative notch in each of the inferior leads). This is highly unlikely to be ATach — because if that upright deflection in lead V1 was a forward-conducting P wave — it would make for an exceedingly long PR interval. This leaves us with a reentry SVT rhythm as the probable diagnosis for ECG #1 (ie, AVNRT or AVRT).
- ECG #2 — shows a regular SVT at ~210/minute. This rate is too fast to be Sinus Tachycardia. It is also too fast to be AFlutter with 2:1 AV conduction — since this would result in an atrial rate = 210 X 2 = 420/minute, which is much faster than the maximum atrial rate for flutter. AFlutter with 1:1 AV conduction is extremely uncommon, and a flutter rate of 210/minute would be uncharacteristically slow unless the patient is on antiarrhythmic therapy. ATach is possible, but in the absence of clear sign of ectopic P waves — ATach is far less likely than a reentry SVT, which is a much more common rhythm. While difficult to prove from this single tracing — I suspect that the RED arrows in ECG #2 (that highlight probable negative deflections in the inferior leads, with sharp angulation in lead V3) represent retrograde atrial conduction with a moderately long RP’ interval (RP' still <PR) that occurs well after the QRS complex (within the latter part of the ST segment).
- ECG #3 (which is Today’s Case) — shows a regular SVT at ~160/minute. There is a slow, gradual upslope to and beyond the ST segment, that leads up to a very deep, negative P wave (highlighted by RED arrows) in front of each of the inferior leads. This deflection before the QRS is positive in lead aVR. P wave negativity in the inferior leads rules out Sinus Tachycardia. Lack of 2:1 atrial activity rules out AFlutter. This essentially leaves us having to decide between ATach (in which case we’d have to postulate huge negative P waves) vs AVNRT in which there is retrograde atrial conduction with a very long RP’ interval (RP' clearly > PR).
PUTTING IT ALL TOGETHER: All 3 tracings in Figure-1 show a regular SVT with retrograde P waves. The KEY to the likely etiology to each rhythm lies with the relative length of the RP’ interval:
- ECG #1 in Figure-1 shows a very short RP’ interval, in which the retrograde P wave distorts the terminal portion of the QRS complex. This is virtually diagnostic of the “slow-fast” form of AVNRT — in which the impulse travels first down the “slow” AV nodal pathway — and back up the “fast” AV nodal pathway. It is because the impulse travels back up (ie, retrograde) over the “fast” AV nodal pathway that the RP’ interval is so short. The “slow-fast” form of AVNRT is by far the most common AVNRT form, so much so that we generally assume “slow-fast” conduction when we simply say “AVNRT”.
- ECG #2 in Figure-1 shows a moderately long RP’ interval. This suggests that there may be an AP (Accessory Pathway) participating in the reentry pathway. Because the AP lies outside of the AV node — the time to circulate around the reentry pathway and conduct back to the atria (retrograde) is longer than when the entire reentry circuit is contained within the AV node. As a result, the retrograde P wave will often be seen to occur within the ST segment, instead of notching the terminal portion of the QRS complex. A follow-up ECG was done in this October 16, 2019 case, and did indeed show WPW.
- ECG #3 in Figure-1 is the 3rd tracing shown from the Today’s Case. It either shows a very long RP’ interval or an Atrial Tachycardia (EP Study pending to determine which). IF this is indeed a very long RP’ interval — then this would be the uncommon “fast-slow” form of AVNRT — in which the impulse travels first down the “fast” AV nodal pathway — and back up the “slow” AV nodal pathway. Retrograde conduction back up the “slow” AV nodal pathway would account for the very long RP’ interval.
PEARL #3 — The BEST way to prove that suspicious deflections are indeed reflective of retrograde atrial conduction during an SVT is to obtain a post-Conversion tracing. This was done in the October 31, 2016 case on Dr. Smith’s ECG Blog:
- For clarity — I’ve reproduced this post-Conversion tracing in Figure-2. The fact that suspicious deflections during the SVT rhythm (RED arrows in ECG #1) are no longer present after conversion to sinus rhythm (BLUE arrows in ECG #1a) proves there was indeed retrograde atrial conduction with a very short RP’ interval in ECG #1. This confirms the diagnosis of the “slow-fast” form of AVNRT.
Illustration of PEARL #2 (discussed earlier) — is evident in Figure-3, in which the laddergram highlights the mechanism in this patient with the “fast-slow” form of AVNRT.
- Note that we see the onset of the tachycardia in Figure-3. After a sinus beat (ie, beat #3) — a PAC (ie, beat #4) initiates the process.
- This PAC presumably finds the slow AV nodal pathway amenable to retrograde conduction at the moment it is traveling toward the ventricles (ie, dotted, slanted lines in the AV nodal tier). IF the timing is “just right” (as it is in Figure-3) — then a reentry circuit utilizing the slow AV nodal pathway (which produces the very long RP’ interval) can be set up.
- I’m uncertain why this “fast-slow” AVNRT terminates after beat #13 (perhaps because the R-R interval of beats #12-13 is a little bit shorter than preceding R-R intervals during the tachycardia?).
- Following 1 sinus beat ( = beat #14) — it looks like the “fast-slow” AVNRT begins again.
MY THEORY for Today’s Case: As discussed above — the principal differential diagnosis for ECG #3 ( = Today’s Case) is between ATach vs the “fast-slow” form of AVNRT. Definitive diagnosis will be made by EP study. I’ve postulated a laddergram for ECG #3. I’ll make the following final points:
- We do not see the onset of the rhythm in Figure-4. This is unfortunate — because it is likely that the onset of this tachycardia would provide a strong clue to etiology of the rhythm.
- A “change” in the rhythm occurs toward the end of the tracing in the form of a PVC. Because AVRT entails reentry involving an AP that lies outside of the AV node — a PVC will be more likely to interrupt the reentry cycle. In contrast — a PVC will be less likely to interrupt a reentry SVT that is contained entirely within the AV node (as occurs with both the “slow-fast” and “fast-slow” forms of AVNRT).
- I’ve drawn the laddergram to illustrate the “fast-slow” form of AVNRT. I suspect this is a more likely etiology for this rhythm than ATach because of the shape of the ST segment (gradually upsloping until the negative inferior P waves — similar to the morphology we see in Figure-3) — and because these negative P waves look huge to be an ectopic atrial focus. That said — ATach can not be ruled out until EP study is done.
 |
| Figure-4: I’ve postulated a laddergram for ECG #3 in Today’s Case (For more on the use of laddergrams — See My Comment in the February 20, 2020 post). |
Our THANKS to Dr. Smith for presenting this case!







Here, one could say "You think the negative deflection in front of the QRS of the ECG #3 above is an inverted P wave. I don't buy that". But the findings during the compensatory pause after a PVC proves that that is what it is as diagrammed in fig 4 above by Dr. Ken Grauer. Another example of "the usefulness of PVCs", one of my favorite ECG topics.
ReplyDeleteK. Wang.
Thanks K! — :)
DeleteA narrow qrs regular tachycardia, mostly asymptomatic, slightly faster than the sinus rate,negative p waves in II, III, AvF, rp>pr ,multiple spontaneous resolution and recurrence - PJRT.
ReplyDeletePJRT occurs predominantly in infants and children — and the patient here is a middle-aged adult ... That said — EP study will tell .. THANKS for your comment Subhasish — :)
DeleteKen...
ReplyDeleteWhat an excellent review! Thank you!
You seemed surprised at the size of the retrograde P waves in the limb leads but I wasn't surprised at all. The P wave amplitude is not dependent on the location of the ectopic pacemaker but on the volume of the atrium and thickness of the myocardial atrial wall. What DID surprise me was the fact that with the reported biatrial enlargement, the P waves weren't any wider than they were. I would have expected some interatrial conduction delay.
The differential diagnosis does appear to boil down to atrial tachycardia or a fast/slow AVNRT. However, I would go with atrial tachycardia strictly on a statistical basis. While it is the least frequent of the three main ectopic narrow-complex tachycardias (AVNRT, AVRT, AT), it is still a lot more common that a fast/slow AVNRT and a heck of a lot more common that a fast/slow AVNRT with a long R-P'. An orthodromic AVRT with a concealed, slowly conducting AP is another possibility, but - as you mentioned (and I agree) - this patient is not someone I would really suspect to have this. It DOES occur in adults, but is seen primarily in those who have just had surgery to correct a congenital heart defect. This patient had no such history.
Thank you again for your diligence in reviewing previous posts and demonstrating the comparisons.
Thanks so much for the kind words Jerry (!) — and for your insights. I completely agree that for “all comers” who present with a regular SVT with suggestion of some atrial activity — ATach is statistically a lot more common than a “fast-slow” AVNRT. BUT — that is not what we are dealing with here. Rather than “all comers” with a regular SVT + suggestion of some atrial activity — ECG #3 (in my Figure-4) is a regular SVT with negative P waves (and to me, a characteristic upsloping shape to the ST segment leading up to those negative P waves) + a long RP’ interval — for which I think statistics favor a “fast-slow” AVNRT. And the PVC further reduces the likelihood that we are dealing with orthodromic AVRT. I could be wrong — and you could be right (!) — and our inability to know for certain until we have EP study results is what makes ECG interpretation so fascinating. THANKS (as always) for your comments Jerry! — :)
DeleteVery informative post. Any EP results yet ?
ReplyDeleteNo. Sorry.
Delete