A man in his early 30s with no significant past medical history was brought to the ED by EMS after being found unresponsive by a friend. EMS arrived and found him awake and alert. He complained of generalized weakness and left lower extremity numbness. He reported that 12 hours prior to arrival he used fentanyl and cocaine. He reported difficulty walking and felt as if his left leg was “asleep.” He denied any chest pain or shortness of breath and stated he felt at his baseline yesterday prior to drug use. On arrival in the ED, he was hypotensive with a systolic blood pressure in the 70s. Fluid resuscitation was initiated.
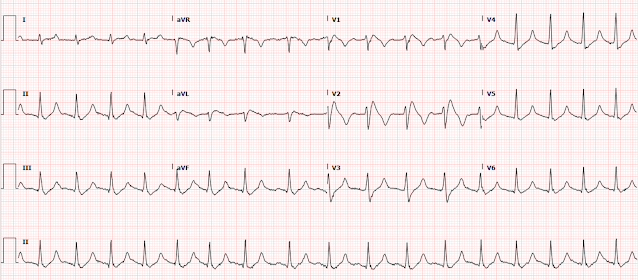
Here is the initial ED ECG:
 |
| What do you think? |
The ECG shows peaked T waves, QRS widening, a coved-type ST segment with inverted T waves most prominent in V1 and V2 consistent with Brugada pattern. ST elevation is also seen in I, II, aVF, and aVL. ST depression is in V3-V6 and aVR.
But of course the leads are misplaced also! There is limb lead reversal, probably LA/RA reversal (see diagram below). You can tell because lead I appears completely inverted, aVR is upright, lead I has a vector opposite of its neighbor lead V6, etc.
-TODAY%20copy.png) |
| From Ken Grauer (See below) — with this Figure adapted from LITFL. |
Despite the clinical context, Cardiology was consulted due to concerns for a "STEMI". They recommended repeating his ECG and awaiting troponin since the patient did not have any chest pain. They opined that the ECG could instead be "metabolic."
Given the initial ECG findings and clinical history, he received 2 gm calcium gluconate due to concerns for hyperkalemia.
Here is the second ECG shortly after the patient received calcium gluconate:
Shortly after repeat ECG, initial high sensitivity troponin I returned elevated at 551 ng/L. (limit of detection = 6 ng/L, URL = 12 ng/L). The second troponin I returned at 699 ng/L. CPK elevated at 50,291 and K returned at 7.9 mE/L. Creatinine elevated at 3.09 mg/dL. Based on his clinical presentation and laboratory findings, rhabdomyolysis was suspected to be the etiology of his hyperkalemia. Cardiology agreed that they thought his ECG findings were metabolic in nature and did not think he needed emergent catheterization despite his rising troponin.
He received several liters of crystalloid and was started on norepinephrine for hypotension and acute renal failure. He also received insulin with D50, sodium bicarbonate, and kayexalate for hyperkalemia.
After initiating treatment for hyperkalemia, repeat ECG showed resolution of Brugada pattern:
The ECG shows sinus tachycardia. The Brugada pattern previously seen in V1 and V2 has almost completely resolved, now actually showing type 2 Brugada morphology in V2 with the wide beta angle. The QRS is narrow and T waves are much less peaked.
He was admitted to the ICU and transferred emergently to a facility where he could undergo emergent dialysis as a part of further evaluation and management. Given his reported left lower extremity pain, numbness, and limited range of motion, orthopedics was consulted. He went emergently to the OR for fasciotomy due to compartment syndrome. A few days later an ECG was repeated which showed normal sinus rhythm with no further hyperkalemia findings:
After a 3-week hospitalization for acute renal failure, hyperkalemia, and compartment syndrome, the patient was discharged to acute rehab.
Learning Points
The diagnosis of OMI is not simply based on the ECG. Clinical context is important, and in cases like this it can be used to help understand the actual pathology.
It is critically important for all EM and critical care providers to have an intimate understanding of hyperkalemia and its ECG findings. Hyperkalemia causes peaked T waves and the "killer B's of hyperkalemia", including bradycardia, broad QRS complexes, blocks of the AV node and bundle branches, Brugada morphology, and otherwise bizarre morphology including sine wave.
Hyperkalemia mimics STEMI and OMI in many distributions, but probably the most common is the Brugada morphology in V1-V2 which mimics anterior OMI for those who cannot recognize the Brugada pattern.
Limb lead reversal can be easily recognized. See the diagram above.
Other cases of hyperkalemia mimicking OMI:
Acute respiratory distress: Correct interpretation of the initial and serial ECG findings, with aggressive management, might have saved his life.
Other cases of limb lead reversal:
A man in his 40s with epigastric pain and a dynamic ECG
ST Elevation in aVL with reciprocal ST Depression in inferior leads and DIffuse ST depression
General hyperkalemia cases:
A 50s year old man with lightheadedness and bradycardia
Patient with Dyspnea. You are handed a triage ECG interpreted as "normal" by the computer. (Physician also reads it as normal)
Is this just right bundle branch block?
A 60-something who has non-specific generalized malaise and is ill appearing.
HyperKalemia with Cardiac Arrest.
Peaked T waves: Hyperacute (STEMI) vs. Early Repolarizaton vs. Hyperkalemia
What will you do for this altered and bradycardic patient?
I saw this computer "normal" ECG in a stack of ECGs I was reading
What is the diagnosis?
Found comatose with prehospital ECG showing "bigeminal PVCs" and "Tachycardia at a rate of 156"
An elderly woman found down with bradycardia and hypotension
A Very Wide Complex Tachycardia. What is the Rhythm? Use Lewis Leads!!
===================================
MY Comment by KEN GRAUER, MD (5/5/2022):
===================================
- Question #1: In the absence of any history — What are the major diagnoses suggested by the ECG in Figure-1?
- Question #2: Is there ECG evidence of acute infarction?
-USE.png) |
| Figure-1: I've reproduced the initial ECG in today's case. |
Regarding the ANSWERS:
Drs. Folk and Meyers have already provided the Answers to the above 2 Questions in their excellent discussion of today's case. These answers are:
- To Question #1 — The ECG in Figure-1 is suggestive of: i) Lead Reversal (apparently from mix-up of the LA-RA electrodes); ii) A Brugada-1 ECG pattern (perhaps Brugada Phenocopy); and, iii) Hyperkalemia (as at least 1 probable factor contributing to the Brugada-1 ECG pattern).
- To Question #2 — This ECG is not suggestive of acute MI.
- By far — the most common lead reversal is mix-up of the LA (Left Arm) and RA (Right Arm) electrodes. As emphasized in Figure-2 — the "tip-off" to LA-RA lead reversal in Figure-1 — is the presence of global negativity (of the P wave, QRS complex and T wave) in lead I.
- In support of our suspicion of LA-RA lead reversal — is the finding in Figure-1 that lead I looks like we expect lead aVR to look — and lead aVR looks like we expect lead I to look.
- Normal R wave progression in the chest leads rules out dextrocardia as the cause of the global negativity in lead I.
-USE.png) |
| Figure-2: Tips for recognizing lead reversal (See text). |
So What Should ECG #1A Look Like?
The presence of lead reversal complicates assessment of what the ECG we are looking at really indicates — especially if the lead reversal isn't recognized promptly enough to immediately repeat the ECG.
- In Figure-3 — I've attached the summary provided above by Drs. Folk and Meyers, to highlight the expected changes brought about by LA-RA lead reversal.
- Can YOU mentally apply this information to the initial ECG in today's case? What should ECG #1A look like?
-USE.png) |
| Figure-3: The initial ECG in the ED — with features of LA-RA lead reversal written below the tracing (See text). |
- This LITFL web page describes the 7 most common lead reversals. There are other possibilities (ie, in which there may be misplacement of multiple leads) — but these are less common and more difficult to predict.
- When I suspect a type of lead reversal that I am less familiar with — I simply review those 7 most common types of lead reversal on the LITFL page — and see if any of the ECG examples they provide seems to apply.
- As noted above — the KEY identifying feature that led me to suspect LA-RA reversal for ECG #1A, was the finding of global negativity of the P wave, QRS complex and T wave in lead I (a result of lead I becoming inverted when the LA and RA electrodes are mixed up).
What ECG #1A Would Look Like:
For Comparison — I've added ECG #1B to the previous Figure to illustrate what the initial ECG in today's case should look like, if the LA and RA electrodes were properly placed (Figure-4):
Returning to My Initial 2 QUESTIONS:
Now that we know what the initial ECG in today's case should look like (ie, ECG #1B in Figure-4) — Let's revisit the 2 Questions that I posed at the very beginning of My Comment:
- LA-RA lead reversal — is confirmed by return of a predominantly upright QRS complex in lead I. There is ST depression — but the T wave is now upright in this lead. And although tiny — the P wave in lead I is also now upright. Finally — the QRS complex in lead aVR is now predominantly negative, as one would anticipate.
- A very typical Brugada-1 ECG pattern — is seen in leads V1 and V2 (See Figure-5 and my discussion below).
- Significant Hyperkalemia — is strongly suggested in ECG #1B because: i) T waves are tall, peaked and pointed in multiple leads (ie, in leads I, aVL; and in V3-thru-V6); ii) The leads in which there is T wave inversion also show pointed negative T waves (PEARL #3 = Awareness that inverted T waves with marked hyperkalemia may also be pointed!); iii) The QRS is widened; iv) Sinus P waves are tiny (soon to become a sinoventricular rhythm, in which despite disappearance of P waves from the ECG — SA node activation persists); and, v) PEARL #4 = Seeing a Brugada-1 ECG pattern is a common manifestation of Brugada Phenocopy — in which the Brugada-1 pattern disappears when serum K+ is corrected). The fact that the Brugada-1 ECG pattern promptly disappeared in today's case after serum K+ normalized — strongly supports the premise that we were seeing Brugada Phenocopy as a result of marked hyperklemia in ECG #1B.
- There is no ECG evidence for acute infarction! — since all ST-T wave changes can be easily explained by the acute renal failure with very high serum K+ = 7.9 mEq/L — which resulted in Brugada Phenocopy with dramatic ST elevation in leads V1,V2. While true that we can not know what ST segments and T waves will look like until serum K+ is corrected — there is no evidence in ECG #1B to suggest acute infarction.
==============================
No matter how many times I have seen Brugada-1 and Brugada-2 ECG patterns — I still find myself referring back to the images in Figure-5:
-USE.png) |
| Figure-5: Review of ECG Patterns in Brugada Syndrome (adapted from the article by Brugada et al in JACC: Vol. 72; Issue 9; 2018) — A) Brugada-1 ECG pattern, showing coved ST-segment elevation ≥2 mm in ≥1 right precordial lead, followed by a negative T-wave. — B) Brugada-2 ECG pattern (the “Saddle-back” pattern) — showing concave-up ST-segment elevation ≥0.5 mm (generally ≥2 mm) in ≥1 right precordial lead, followed by a positive T-wave. — C) Additional criteria for diagnosis of a Brugada-2 ECG pattern (TOP: the ß-angle; BOTTOM: A Brugada-2 pattern is present if 5 mm down from the maximum r’ rise point — the base of the triangle formed is ≥4). |
- A Brugada Type-1 ECG pattern is diagnosed by the finding of ST elevation of ≥2 mm in one or more of the right precordial leads (ie, V1, V2, V3) — followed by an r’ wave and a coved or straight ST segment — in which the ST segment crosses the isoelectric line and ends in a negative T wave (See Panel A in Figure-5).
- A Brugada-1 pattern may either be observed spontaneously (with leads V1 and/or V2 positioned normally — or positioned 1 or 2 interspaces higher than usual) — or — a Brugada-1 pattern may be observed on provocative drug testing after IV administration of a sodium-channel blocking agent such as ajmaline, flecainide or procainamide.
- NOTE: In the past, the diagnosis of Brugada Syndrome required not only the presence of a Brugada-1 ECG pattern — but also a history of sudden death, sustained VT, non-vasovagal syncope or a positive family history of sudden death at an early age. This definition was changed following an expert consensus panel in 2013 — so that at the present time, all that is needed to diagnose Brugada Syndrome is a spontaneous or induced Brugada-1 ECG pattern, without need for additional criteria.
- Panel B in Figure-5 illustrates the Brugada Type-2 or “Saddle-back” ECG pattern. This pattern may be suggestive — but is not diagnostic of Brugada Syndrome. As per Drs. Folk and Meyers — the prominent Brugada-1 ECG pattern that was noted in leads V1,V2 of the first 2 ECGs in today's case — regressed to the remnants of a Brugada-2 pattern (showing no more than a small r' with wide ß-angle) in the 3rd ECG, which was recorded after hyperkalemia was treated.
- PEARL #5: A number of conditions other than Brugada Syndrome may temporarily produce a Brugada-1 ECG pattern. These include (among others) — acute febrile illness — variations in autonomic tone — hypothermia — ischemia/infarction/cardiac arrest — and Hyperkalemia. Patients with such conditions that may transiently mimic the ECG findings of a Brugada-1 pattern are said to have Brugada Phenocopy. The importance of being aware of this phenomenon of Brugada Phenocopy — is that correction of the underlying condition (ie, hyperkalemia in today’s case) may result in resolution of the Brugada-1 ECG pattern, with a much better prognosis compared to patients with true Brugada Syndrome.
==============================
- The July 29, 2018 post (LA-RA reversal).
- The February 11, 2020 post (LA-RA reversal).
- The March 18, 2020 post (LA-RA reversal).
- The November 27, 2021 post (LA-RA reversal).
- The June 4, 2018 post (LA-LL reversal).
- The August 28, 2020 post (LA-LL reversal).
- The November 19, 2020 post (LA-LL reversal).
- The November 4, 2018 post (Leads V1,V2 placed too high).
- The April 17, 2022 post (Leads V1,V2 placed too high).
==============================



.png)
-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.