Written by Pendell Meyers with edits by Smith
NOTE: Please check out My Comment at the very bottom of this post — in which I amplify discussion by Drs. Meyers & Smith on some subtle-but-important ECG findings on the initial ECG — Ken Grauer, MD —
A man in his 60s called EMS apparently for shortness of breath. EMS found him in distress and hypoxemic requiring 4 L nasal cannula to maintain oxygen saturation greater than 93%.
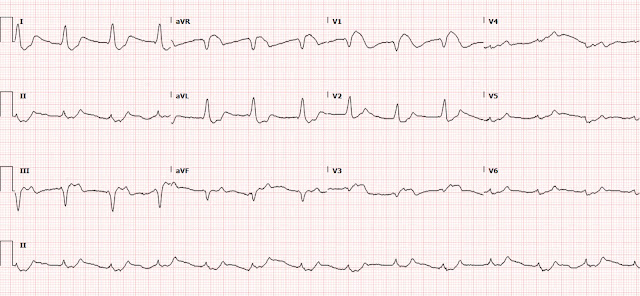
Here is his triage ECG:
 |
| What do you think? |
An old ECG was available on file, from 2 years ago:
 |
| RBBB, otherwise normal. |
The triage ECG is diagnostic of life threatening hyperkalemia (sodium channel blockade would also produce this pattern, but the patient was not known to be on any sodium blocking medications). There is the very common brugada pattern STEMI mimic seen in V1 and partially in V3 and aVR. There is also STE in III with reciprocal STD in I and aVL which is due to the hyperkalemia.
When hyperkalemia causes STEMI mimics, in my experience, the most common areas where the false positive STE morphology is located are, in this order: right precordial leads (due to brugada morphology), inferior leads (as seen here), and then the high lateral leads. We have many such cases on the blog, see links below.
This ECG is easy for those who have been taught this hyperkalemia pattern, and almost impossible to understand for those who haven't.
Unfortunately, the providers interpreted this ECG as a "STEMI" and activated the cath lab. The interventionalist called the ED provider and completely agreed that the ECG represented STEMI. However, they informed the ED team that the patient's size was not physically compatible with the cath lab table, and thus could not be cathed. Instead, the interventionalist recommended thrombolytics.
Tenecteplase was given immediately.
At this time, the patient was still in respiratory distress; he was placed on noninvasive positive pressure ventilation, with intact mental status.
Soon afterwards, the initial labs returned:
K 8.3 mEq/L
Na 125 mEq/L
Creatinine 9.41 mg/dL
High sensitivity troponin I returned at 6 ng/L (99% URL for men less than 20 ng/L)
The patient was given 10 mg albuterol nebulized, 2 gm calcium gluconate IV, 10 U regular insulin, D50, and 50 mEq sodium bicarbonate.
Meyers comment: this is all reasonable initial therapy, except that 2 gm calcium gluconate will not be enough. Remember that a "normal" initial dose of CaCl is 1 gm, which contains the same amount of elemental calcium as 3 gm of calcium gluconate. You must immediately reevaluate the QRS width and overall morphology and administer more and more calcium until you titrate to normal QRS and absence of dramatic brugada morphology. See cases below where we needed huge amounts of calcium every 20 minutes to keep the patient out of arrest and with a reasonable QRS, up to a total of as much as 24 g of calcium gluconate (or 8 g of CaCl), and more is NOT contraindicated, if necessary.
Transfer was initiated to the tertiary care center with cardiology, nephrology, and ICU services.
He required constant noninvasive positive pressure ventilation for respiratory support.
Low dose norepinephrine was added for hypotension.
Just before transport to tertiary care facility, around 2 hours after initial presentation, the potassium was re-measured at 8.4 mEq/L.
Then the patient received another dose of albuterol 10 mg, Ca gluconate 2 gm, insulin 10 U, and sodium bicarbonate 50 mEq soon after that measurement, before transport.
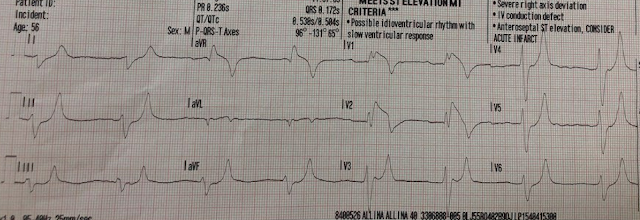
He arrived at the ICU and had another ECG recorded:
 |
| No significant change, thus no significant progress. |
Potassium was re-measured at 8.4 mEq/L. The second troponin returned at 17 ng/L (same assay as above).
Again given: Ca gluc 2gm, regular insulin 5U, and sodium zirconium cyclosilicate 10 gm are given.
2 hours later, the ECG was almost exactly the same, with no progress made.
Before a dialysis catheter could be placed, the patient had deterioration in mental status and required intubation. He experienced peri-intubation cardiac arrest and could not be resuscitated.
Learning Points:
The difference between OMI and hyperK can be deadly. In other words, memorizing the patterns of OMI and hyperK mimics can potentially save lives and prevent false positive administration of thrombolytics or cath lab activation.
The onus is on Emergency Medicine to be the ones who master the ECG, because we see all the emergent, undifferentiated patients with ACS symptoms, from whom we must recognize the "needles in the haystack" who have OMI, hyperkalemia, and differentiate them from benign chest pain and dyspnea, and all sorts of OMI mimics. At least in the US model, the cardiologist does not see these other patients, and cannot possibly have as much experience with OMI mimics as Emergency Medicine.
Brugada pattern STE is (I believe) the most common OMI mimic caused by hyperkalemia. Inferior leads and high lateral leads have also been described as in cases below. The typical hyperK mimic of OMI has a large R-wave, with STE, in V1, V2, and aVR, with a wide QRS, along with a variety of other findings.
In addition to peaked T waves, hyperkalemia causes what I call the "killer B's" of hyperkalemia: Broad (QRS widening), Brady (bradycardias of all varieties), Blocks (AV blocks, bundle branch blocks), Brugada (pattern), and Bizarre (bizarre morphology, sine wave, etc.).
There is no maximum dose of calcium when the patient is at risk of death from severe hyperkalemia. From my observation of many providers who are not experienced with deadly hyperkalemia, the administration of calcium is often a simple question of "yes or no" or a "checkbox." It is not enough to administer a dose of calcium and wait until the next chemistry panel results. You must titrate the calcium until you have achieved a narrow QRS with an absence of brugada morphology or other dramatic hyperkalemic findings.
Cases of hyperkalemia mimicking OMI:
"Steve, what do you think of this ECG in this Cardiac Arrest Patient?"
 |
General hyperkalemia cases:
A 50s year old man with lightheadedness and bradycardia
Patient with Dyspnea. You are handed a triage ECG interpreted as "normal" by the computer. (Physician also reads it as normal)
Is this just right bundle branch block?
A 60-something who has non-specific generalized malaise and is ill appearing.
HyperKalemia with Cardiac Arrest.
Peaked T waves: Hyperacute (STEMI) vs. Early Repolarizaton vs. Hyperkalemia
What will you do for this altered and bradycardic patient?
I saw this computer "normal" ECG in a stack of ECGs I was reading
What is the diagnosis?
Found comatose with prehospital ECG showing "bigeminal PVCs" and "Tachycardia at a rate of 156"
An elderly woman found down with bradycardia and hypotension
A Very Wide Complex Tachycardia. What is the Rhythm? Use Lewis Leads!!
===================================
MY Comment by KEN GRAUER, MD (1/16/2022):
===================================
Superb ECG Blog post by Drs. Meyers & Smith on some of the life-threatening but less easily recognizable forms of hyperkalemia.
- WHY are these cases “less recognizable” for potentially life-threatening hyperkalemia?
ANSWER: Because we don’t see the very tall, peaked T waves with slender base that we are looking for ...
QUESTION: WHY should these cases be more recognizable than they are to emergency care providers?
ANSWER: Because in addition to tall, peaked (and pointed) T waves with a narrow base — there are a series of additional ECG findings to look for. For clarity — I’ve labeled the initial ECG in today’s case (Figure-1). Features of life-threatening hyperkalemia that should be evident on this tracing include the following:
- Brugada phenocopy pattern in lead V1 (as emphasized above by Drs. Meyers and Smith).
- QRS widening in a pattern that does not resemble any known form of BBB.
- Either extremely tiny P waves (vertical BLUE lines in the long lead II rhythm strip in Figure-1) — or — no P waves at all (ie, sinoventricular rhythm).
- Subtle-but-real T wave peaking (RED arrows).
 |
| Figure-1: I've labeled the initial ECG in today's case (See text). |
Comment:
We all know to look for hyperkalemia in patients predisposed to developing this electrolyte disorder (ie, acute or chronic renal failure; severe acidosis; use of potassium-retaining medications; severe trauma, etc.). Recognition is much easier when one of these “predisposing” conditions is present.
- But almost all of the patients emergency providers see (ie, in-the-field when EMS is called — or in the Emergency Department) are potentially very ill, and therefore potentially “predisposed” to developing hyperkalemia.
So WHAT is the Rhythm in Figure-1?
As a reminder of WHY determination of the cardiac rhythm can be so challenging when there is significant hyperkalemia — I've added Figure-2.
- In today's case — I fully acknowledge that I do not know for certain what the rhythm in Figure-1 is. I suspect that the vertical BLUE lines that I've drawn under the long lead II rhythm strip indicate placement of tiny P waves with a prolonged PR interval — BUT — it could also be that there are no P waves — in which case this would either be junctional or sinoventricular rhythm.
- Practically speaking — it does not matter what the rhythm in Figure-1 is — because IF this patient would be promptly treated with Calcium — whatever this rhythm was would most probably rapidly resolve.
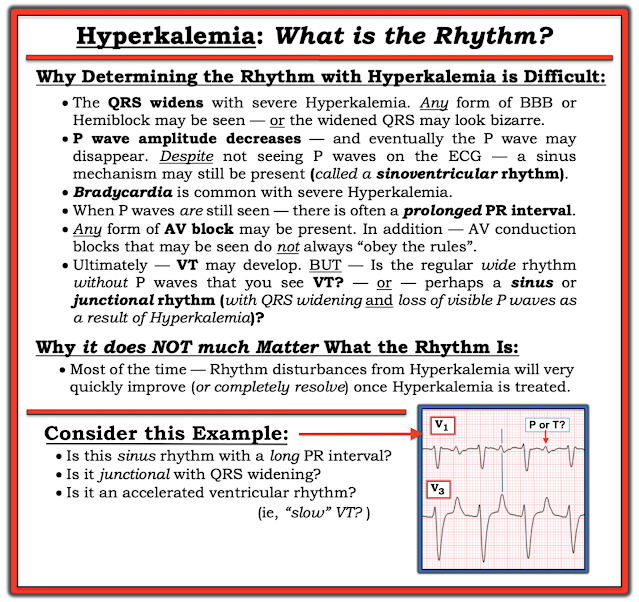 |
| Figure-2: Reasons why determining the rhythm with severe hyperkalemia is so challenging. |
BOTTOM LINE: I believe the BEST way not to overlook potentially life-threatening hyperkalemia is to: i) Always consider it in the acutely ill patients you see; ii) Look not only for tall, peaked T waves — but ALSO for:
- Unexpected bradycardia.
- Small (or absent) P waves.
- 1st-degree AV block (often with markedly prolonged PR intervals).
- Other forms of AV block (that often do not obey the "usual rules” of AV block).
- QRS widening (especially if QRS morphology is not in a pattern of a known form of BBB).
- Unexplained marked right axis in the frontal plane.
- Brugada phenocopy patterns.
- More subtle forms of T wave peaking (ie, as seen in Figure-1 — in which although small and not pointed — many T waves are surprisingly more “peaked” than you would expect them to be given how small the QRS is, and how otherwise flat the ST segments are).
For MORE on Hyperkalemia:
- CLICK HERE — for review of the "textbook" sequence of ECG findings with hyperkalemia.
- CLICK HERE — to listen to my 8-minute Audio on Pearls for ECG Recognition of Hyperkalemia.












No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.