A 90-something year old woman presented with an acute mild stroke.
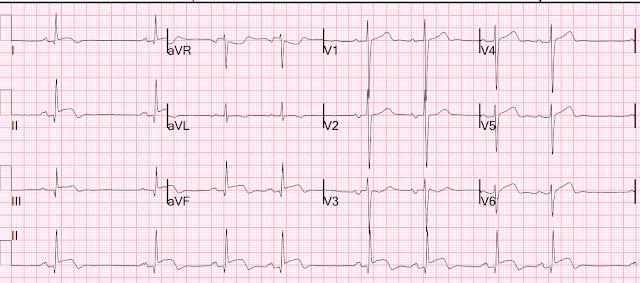
She had a routine ECG as part of her workup:
This was shown to me in real time.
I thought it had to be an inferior-lateral-posterior OMI. But the patient had no symptoms. Later, she did admit to some vague chest discomfort, but that could be due to the power of suggestion.
The one strange thing that I noted at the time is that there is no reciprocal ST depression in aVL. This is extremely unusual in inferior OMI, even if there is simultaneous STE in V5-6.
We studied this: In this paper on the importance of lead aVL for diagnosis of inferior OMI, we reported that all 33 patients with inferolateral MI, as manifested by STE in V5 and V6, still had ST depression in aVL. V5 and V6 are caudal to aVL and so an inferior ST vector towards lead aVF is also slightly towards V5 and V6 but away from aVL!! So V5 and V6 will have some ST elevation while aVL has ST depression. Thus, even inferolateral MI has reciprocal ST depression in aVL.
The cath lab was activated.
First trop = 42 ng/L (URL for women = 16, but for a 90-something, it is likely that the URL is much higher)
The angiogram was negative!
Peak trop 62 ng/L (would be very low for acute OMI)
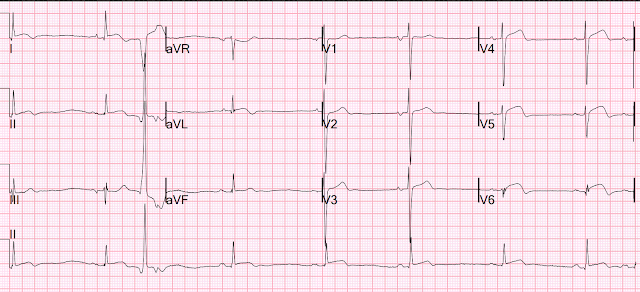
Next AM ECG:
Still with very ischemic looking T-waves.Later, I found old ECGs:
5 month prior in clinic:
9 months prior in clinic with no chest symptoms:
1 year prior in the ED with chest pain:
For this ECG and chest pain in the ED, the Cath lab activated. But the angiogram was clean. There was no OMI. Peak hs troponin I = 75 ng/L
4 years prior in ED with chest pain:
Indeed, this one was really an RCA OMI with peak troponin of 59,000 ng/L
This is the post PCI ECG at 4 years prior:
What is going on?
It turns out that she has hypertrophic cardiomyopathy.
The diagnosis was a bit hard to find in the chart, and the echocardiogram did only stated "assymetric hypertrophy."
Here is the echo report from one year prior to this visit:
Normal to hyperdynamic LV ejection fraction, 70%
Left ventricular hypertrophy, asymmetric.
Regional wall motion abnormality-distal septum and apex.
Regional wall motion abnormality-basal inferior akinetic .
Here is the echo report for this visit (after the negative angiogram):
Hypertrophic cardiomyopathy with asymmetric septal hypertrophy.
Normal LV cavity size and systolic function.
The estimated left ventricular ejection fraction is 60 %.
No left ventricular out flow obstruction at rest or with valsalva.
Regional wall motion abnormality-apical septum, apical anterior, apical
inferior, and apex, dyskinetic.
Learning Points:
1. When something doesn't fit, look carefully through the patient's chart. You might find the explanation.
2. Always look at old ECGs, even if you think the diagnosis is obvious.
3. Use the Queen of Hearts. If she is not highly confident, something might be wrong (see below)
I put that top one through the Queen of Hearts AI app:
The Queen had low confidence for OMI. She knew something that we humans did not.
Here she explains her interpretation:
MY Comment, by KEN GRAUER, MD (11/11/2023):
- My Thoughts on the 12-Lead: "Very interesting! I'd really want to know the age of the patient and some history. Although there is inferior lead ST elevation — this is unlike a typical inferior OMI in that there is also ST elevation in lead I and slight ST elevation in lead V1."
- My Rationale: I didn't think this ECG fit any of the "usual patterns". The inferior Q waves with hyperacute-looking elevated ST segments with terminal T wave inversion clearly suggested acute inferior OMI. But the usual "reciprocal" (mirror-image opposite) ST-T wave picture that is almost always seen in lead aVL with acute inferior MI was lacking (ie, No ST depression with no more than minimal T inversion in aVL) — and — I don't think I've ever seen ST elevation in lead I with acute RCA occlusion. I wouldn't expect ST elevation in lead V1 if there was LCx occlusion.
- Additional Observations re ECG #1: There is poor R wave progression. Instead — there are deep anterior S waves (ie, 20-25 mm in leads V1,V2) — as well as a prominent initial R wave in lead V1 and surprisingly tall ( =10 mm) R wave already by lead V2 — suggesting at the least LVH, and possible increased septal forces.
- My Initial Thoughts on the Rhythm: The rhythm is bizarre! There appears to be group beating — which with acute inferior OMI almost always indicates Mobitz I 2nd-degree AV block ( = AV Wenckebach) — but the rhythm in ECG #1 is not AV Wenckebach because: i) The atrial rhythm is not regular (as it should be with AV Wenckebach — or with SA Block except for the interval with the blocked P wave); — ii) The PR interval is not increasing; and, iii) True "Wenckebach Periodicity" is lacking — in that although the R-R interval does progressively decrease in the grouping of beats #2,3,4 — it does not do so for the grouping of beats #5,6,7,8 (and the pause between beats #6-7 seems too short for these last 4 beats to represent 2 Wenckebach cycles).
- My Overall Impression of ECG #1: A bit bizarre — but although this ECG does not fit the usual pattern of acute inferior OMI — given ST elevation in the inferior leads, as well as in leads V5,V6 — an acute OMI needs to be assumed until this is ruled out. That said, despite the group beating — the rhythm is not consistent with AV Wenckebach. I added, "Makes me wonder if this could be myocarditis in a younger adult — maybe even with sinus arrhythmia."
-USE.png) |
| Figure-1: The initial ECG in today's case. |
- Review of the patient's chart showed evidence of prior RCA OMI 4 years earlier.
- That said — I found my review of prior tracings on this patient (as shown above by Dr. Smith) — made it difficult to know which (if any) of the ST-T wave changes in ECG #1 might be acute.
- There was a question in the record of hypertrophic cardiomyopathy ...
- That said — Learning that today's patient was 90 years old (!!!) — and seeing evidence of bradycardia (primarily sinus arrhythmia with some ectopic atrial activity) on prior tracings — suggested to me that this patient probably has SSS (Sick Sinus Syndrome), though not yet needing a pacemaker — and that the rhythm in ECG #1 is most likely more of the same that is seen on prior tracings = sinus bradycardia and arrhythmia (and not any form of AV block).
- Re the ECG findings in HCM (Hypertrophic CardioMyopathy) — See My Comment at the bottom of the page in the October 28, 2023 post in Dr. Smith's ECG Blog.
- Re the common occurrence of Mobitz I (AV Wenckebach) with acute inferior MI — See My Comment at the bottom of the page in the July 30, 2023 post.
- Re ECG recognition of SA Block — See My Comment at the bottom of the page in the May 25, 2022 post — as well as my comment in the Addendum of the August 30, 2023 post.








No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.