Sent by anonymous, written by Pendell Meyers
A man in his 60s presented with acute chest pain with diaphoresis. He had received aspirin and nitroglycerin by EMS, with some improvement. His vitals were within normal limits. Here is his triage ECG:
 |
| What do you think? |
 |
 |
| This ECG is normal, and thus confirms the concerns explained above. |
 |
| Inferoposterior (and lateral V5-6) reperfusion findings. T-wave inversion in inferior and lateral leads Reciprocally upright T-wave in aVL and V2 |
 |
| Ongoing reperfusion. |
Repeat troponins:
21,781 ng/L
22,818 ng/L
No further troponins were measured.
No further ECG were ever recorded.
Cath done around 4pm next afternoon:
Acute culprit lesion: LCX 99%, TIMI 1 flow, stented
Also LAD 50%, TIMI 3 flow, which was also stented
And chronic RCA occlusion with collaterals (no information is in the cath report regarding where the collateral flow is from, for example if collateral flow was from the LAD or LCX).
Echo:
EF 40%
Moderate hypokinesis of the posterolateral myocardium
Learning Points:
OMI can be subtle, yet diagnostic.
Sometimes hyperacute T waves are more easily recognized as hyperacute when compared with prior available ECGs.
In the context of ACS, ST depression maximal in V1-V4 (rather than V5-V6) not due to a QRS abnormality is specific for posterior OMI.
At least half of LCX OMIs are missed. We know that NSTEMIs with delayed OMI management suffer almost double the short and long-term mortality of NSTEMIs without OMI.
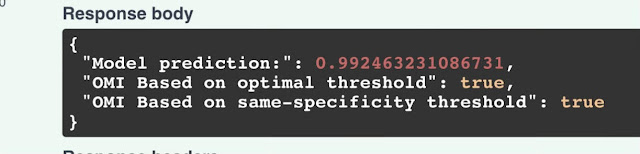
Artificial intelligence can be trained to recognize subtle OMI
- Given the history of new chest pain with diaphoresis in this 60ish year old man — the diagnosis of acute OMI should not have been missed from the initial ECG.
- As per Dr. Meyers — Concerns raised by the ECG findings in ECG #1 — were clearly confirmed by comparing this initial tracing with the prior ECG.
- The follow-up ECG (done ~6 hours after ECG #1) — supports my suspicion regarding the physiologic sequence of events in today's evolving OMI (and provides the likely explanation for why frank ST elevation was not seen in ECG #1).
- As emphasized numerous times in Dr. Smith's ECG Blog — the onset of acute coronary occlusion typically corresponds to the onset of ST elevation in the anatomic area served by the "culprit" vessel.
- Spontaneous reopening of the acutely occluded artery may occur prior to active treatment. This spontaneous reperfusion is typically accompanied by symptom relief (or at least reduction in chest pain severity) — and — return of elevated ST segments toward the baseline.
- With a modicum of time — reperfusion ST-T wave changes occur (typically in the form of T wave inversion in leads that showed ST elevation).
- Because posterior OMI is recognized by chest lead ST depression that is maximal in leads V2-V4 — reperfusion ST-T wave changes of posterior OMI typically result in increased T wave positivity in those leads that showed ST depression.
- The fact that this patient's chest pain decreased after receiving NTG from the EMS team — should suggest that it would not be surprising if ST-T wave changes were relatively modest on this patient's 1st ECG in the ED (ie, chest pain reduction following NTG possibly signaling the beginning of spontaneous reperfusion). Our expectations would be different — IF instead, this patient's chest pain was increasing as the initial ECG was recorded (in which case we would expect further increase in acute ST-T wave changes on the next ECG).
- Had the initial interpreter of today's ECG appreciated the above physiologic sequence of events — they would have repeated the initial ECG within no more than 15-20 minutes (instead of waiting ~6 hours before doing so). Given how modest the amount of ST segment deviation is in ECG #1 — it would not have been at all surprising to see ongoing reperfusion ST-T wave changes in a repeat ECG done within 15-20 minutes after ECG #1 — in which case, the presence of "dynamic" (ie, evolving) ST-T wave changes would have confirmed an acute event almost 6 hours before the 2nd ECG was finally done.
- Cardiac cath was not done until 4pm the following day. Because an acutely occluded vessel that has spontaneously reperfused — may just as easily reocclude — prompt cardiac cath with PCI was indicated in today's case any time after ECG #1 was done. The fact that it was delayed until late the next day is further indication that the treating team failed to appreciate the physiologic sequence of events associated with evolving OMI.
-USE.png) |
| Figure-1: Comparison of the first 3 ECGs in today's case. |
- There is sinus tachycardia at 100-105/minute. Axis and intervals are normal. There is no chamber enlargement. There is a tiny q wave in lead aVL. R wave progression is normal — with transition (where the R wave becomes taller than the S wave is deep) occurring normally between leads V3-to-V4.
- The most "eye-catching" ST-T wave abnormality is in lead V2. As we often emphasize — the ST segment is so very often slightly elevated in anterior leads V2 and V3. The fact that if anything, there is slight ST depression in lead V2 is clearly abnormal in a patient with new chest pain. The scooped shape of this ST depression in lead V2 makes for a positive "Mirror" Test (For my thoughts on the Mirror Test — See My Comment in the September 21, 2022 post in Dr. Smith's ECG Blog).
- There is also subtle-but-real ST depression in leads V3 and V4.
- Rather than seeing normally positive T waves in lateral chest leads V5 and V6 — the T waves in these leads are flatter-than-they-should-be. Thus, there is V1-V6 T Wave "Imbalance" (ie, When all chest lead T waves are positive — the T wave in lead V6 is generally more positive than the T wave in lead V1 — which is not the case in Figure-1). As I emphasize in My Comment at the bottom of the page in the June 1, 2022 post — by itself, this V1-V6 "T wave imbalance" is a nonspecific finding. But in the context of a patient with new chest pain, whose ECG shows a series of other worrisome ECG findings — this is one more indication of a potential acute event.
- In the context of the above chest lead findings in ECG #1 — the straightening of the ST segment takeoff in each of the inferior leads is not normal — and suggests a probable hyperacute change. This suggestion is strengthened by the mirror-image opposite (reciprocal) ST-T wave picture in lead aVL (compared to the ST-T wave in lead III). If we also consider that the ST-T wave flattening in lead I is not normal — this makes for subtle-but-real ST-T wave changes in 11/12 leads in ECG-1!
- We unfortunately do not know the circumstances under which this prior ECG #2 was obtained. That said, as emphasized by Dr. Meyers — there should be no doubt from lead-to-lead comparison between ECG #1 and ECG #2, that the above described findings in ECG #1 are acute!
- The history can be helpful. Although we are missing details on the timing of chest pain severity in today's case — it seems logical that the reason ST-T wave deviations in the initial ECG were so modest, is that corresponding with the patient's reduced chest pain after NTG — spontaneous reperfusion had begun.
- ECG findings in ECG #3 support the likelihood of ongoing reperfusion because: i) ST depression in leads V2-V4 has resolved; ii) Increased T wave positivity is now seen in leads V1-thru-V3 (suggesting posterior wall reperfusion); iii) The hyperacute ST segment takeoff in each of the inferior leads has now been replaced by flat ST segments with T wave inversion (consistent with inferior wall reperfusion); and iv) ST segment flattening in lead I and reciprocal T wave inversion in lead aVL that was seen in ECG #1 — has been replaced by T wave positivity in these 2 high-lateral leads (consistent with reciprocal changes from inferior wall reperfusion).
- If there is any doubt about whether an acute process might be evolving — repeat the ECG! Continue to repeat the ECG as often as needed until you are certain about what is happening.
- All-too-often ignored (and not recorded) — is careful correlation of the presence and severity of chest pain — to each ECG that is recorded. Attention to this correlation tells a "story" — and helps to interpret each ECG by telling you the stage in the pathophysiologic process of OMI evolution.
- Even AI can be taught to recognize subtle acute OMI ...

No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.