This was texted to me by a former resident, with no information:
What do you think?
Here Ken Grauer has used the PM Cardio app to improve the image:
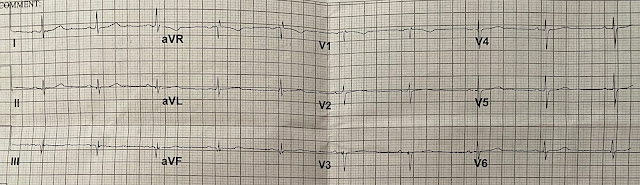
This was my immediate response: "Acute proximal LAD OMI" To me it is obvious and diagnostic.
There are hyperacute T-waves in I, aVL, V2-V6. These are wide, bulky, with large area under the curve relative to the QRS size.
Furthermore, there is a QS-wave in V3 and qrS in V4, both diagnostic of MI at some time (past or present). We have shown here and validated here that old MI has relatively small T-wave (by amplitude). In this situation (QS-waves), a T/QRS ratio >0.36 in any of V1-V4 is highly specific for ACUTE MI.
The former resident then wrote this: "All my colleagues are amazed that I diagnosed this pretty obvious OMI immediately. I didn’t think it was subtle at all but they all say it is."
To my former resident it was also obvious and diagnostic.
He immediately activated the cath lab.
I wish I knew how many clinicians would recognize this diagnostic ECG, and how many would not.
Then because he knew there was LAD Occlusion, he suspected that there might be evolution, so he recorded this one 7 minutes later:
This shows obvious evolution. But although it is always a good idea to get serial ECGs, they do not always show evolution, and when they do, it is not always this rapid. So don't let absence of evolution stop you from activating the cath lab with the first ECG.
He also found this previous one:
Later, he provided this info: A 60-something woman with a history of MI and PCI, with 3 hours of chest discomfort.
The initial hs troponin was 53 ng/L. This troponin value makes the diagnosis of acute MI almost certain, but this troponin by no means tells you if it is OMI or Non-OMI (NOMI). Only the EKG can tell you OMI or Non-OMI. (It is clearly not a STEMI and is therefore a Non-STEMI or NSTEMI.)
Angiography confirmed LAD OMI and thrombus.
This shows that the term Non-STEMI is useless, as Non-STEMI can be either OMI or NOMI.
On the other hand, a positive troponin like that with ongoing chest pain, even in the absence of any ECG findings of Acute MI or OMI, is an indication for the cath lab.
It is remarkable that some interpreters can see this ECG as Obvious and Diagnostic, while others see nothing at all.
This is why I often say that "It is not the ECG which is non-specific; it is the interpreter who is non-specific"
The ECG holds an immense amount of information which is not seen by many humans. Probably, much of the information is not seen by ANY human. We are hoping that artificial intelligence will find aspects of the ECG that are clues to OMI that we have never even suspected. These might be anything from QRSTU morphologies to rhythm irregularities, including beat to beat variability, QT interval, or anything else.
It may even be found that single lead ECG holds information on OMI that we have not yet suspected. Wearables such as Apple watch may some day be able to diagnose OMI.
What is needed is to feed the AI algorithms huge numbers of tracings with verfiable outcomes. The latter is the difficult part: it is very hard to determine, even in retrospect, what the state of the artery was at the time of the tracing.
==================================
My Comment by KEN GRAUER, MD (1/2/2023):
==================================
I liked today's case — because a definitive answer is forthcoming within seconds. In a patient with new symptoms — there should be no doubt from the initial tracing that the cath lab should be immediately activated.
- For clarity and ease of comparison in Figure-1 — I've put the 3 tracings in today's case together.
My Thoughts on the Initial ECG:
There is low voltage in ECG #1. The rhythm is sinus at ~85-90/minute. All intervals (PR, QRS, QTc) are normal. The axis is leftward — but not enough to qualify as LAHB, as the QRS is not predominantly negative in lead II. Regarding Q-R-S-T Changes:
- Q waves are present in each of the inferior leads. But more than simply being Q waves — there is extra fragmentation in these leads (ie, following the initial Q wave — a small R wave is seen, only to be aborted by terminal S waves in each of the inferior leads). This fragmented Q wave appearance — especially given the relative width of the Q waves in leads III and aVF of ECG #1 (considering the tiny size of the QRS in these leads) — is virtually diagnostic of inferior MI at some point in time. But this is not necessarily an acute change (and it is not the "diagnostic" feature in today's case).
- Abnormal Q waves are also present in the chest leads of ECG #1. Following the QS in lead V1 — a small-but-definite initial r wave is seen in lead V2. There is then loss of R wave, as a QS complex is seen in lead V3. We once again see a fragmented Q wave in lead V4 (ie, a tiny initial negative deflection — followed by a small positive r wave, before ending with a predominant S wave). This poor R wave progression (with loss of R from V2-to-V3 — and fragmented Q in V4) — is consistent with anterior MI at some point in time (but once again — this is not necessarily an acute finding).
The Reason ECG #1 is Diagnostic = ST-T Wave Changes
The point to emphasize is that in a patient with new symptoms — the abnormal appearance of ST-T waves in ECG #1 is absolutely diagnostic of acute OMI until proven otherwise:
- No less than 8/12 leads in ECG #1 show hyperacute T waves. As emphasized in numerous posts on Dr. Smith's ECG Blog — in a patient with new symptoms, hyperacute T waves are suggested by a "hypervoluminous" appearance — in which T waves are taller than expected (given the amplitude of the QRS in the respective lead) — as well as T waves being "fatter"-at-their-peak and wider-at-their-base than should be expected.
- The most obvious hyperacute T waves in ECG #1 — are seen in leads I and aVL (given the tiny size of the QRS in these leads) — as well as in leads V2-thru-V6.
- Given its position next to lead I — I interpreted the taller-than-expected T wave in lead II (that exceeds the amplitude of the R wave in this lead) — as also being hyperacute.
- KEY Point: The reason we absolutely know that T waves in the above cited 8 leads are acute — is the presence of reciprocal changes in leads III and aVF of ECG #1. Specifically — the wide, rounded T wave inversion seen in lead III is a virtual mirror-image of the hyperacute T wave in lead aVL. In lead aVF — the ST segment is uncharacteristically flat, which is clearly an abnormal change.
- BOTTOM Line: Although the ST-T wave changes in ECG #1 do not satisfy millimeter ST elevation criteria for a STEMI — in a patient with new symptoms, the finding of multiple hyperacute T waves with inferior lead reciprocal ST-T wave changes should immediately prompt activation of the cath lab.
-USE%20copy.png) |
| Figure-1: The 3 ECGs in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
The Repeat ECG:
If doubt exists on seeing the initial ECG in a patient with new symptoms (OR — if there may be need to convince a reluctant cardiologist of the need for acute cath) — then repeat the ECG!
- Today's case provides an impressive example of how quickly things can change during an acutely evolving OMI (ie, ECG #2 was obtained just 7 minutes after ECG #1!).
- The major change in ECG #2 — is that the ST segment takeoff has straightened, and is elevating in each of the chest leads that showed hyperacute T waves in ECG #1 (ie, in leads V2-thru-V6). This dramatic evolution-in-progress confirms a large ongoing acute infarction.
The Prior Tracing:
Availability of a prior (baseline) ECG — may sometimes provide assistance in confirming that ST-T wave changes on an initial ECG are indeed acute. While the prior ECG was not needed for diagnosis in today's case (because the ST-T wave changes in 10/12 leads in ECG #1 were so obviously acute) — it is nevertheless insightful to compare the initial ECG with this patient's baseline tracing.
- Note that the fragmented inferior lead Q waves — as well as the loss of R wave from lead V2-to-V3 — were both present on the prior tracing. This suggests that this patient did indeed have a previous inferior and anterior lead event.
- The overall low voltage was also present on the prior tracing.
- The most remarkable change between ECG #3 and today's initial ECG — is that ST-T waves were previously diffusely flattened. This confirms that the hyperacute and reciprocal ST-T wave changes that I noted above in 10/12 leads of ECG #1 were indeed all acute!


-USE%20copy.png)

No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.