A woman in her late 20s with a past medical history of cervical cancer status post chemotherapy and radiation therapy presented to the emergency department for shortness of breath, chest tightness, and two episodes of syncope.
Her initial vital signs revealed a temp of 97.7F, HR 125, RR 20, BP 115/90, and an oxygen saturation of 95% on room air. Upon arrival, she did not appear in acute distress. She was noted to be tachycardic and her heart sounds were distant on physical exam. She had a normal respiratory effort, and her lungs were clear to auscultation bilaterally.
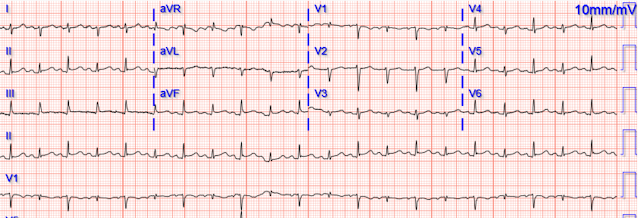
Given her reported chest pain, shortness of breath, and syncope, an ECG was quickly obtained:
The ECG shows sinus tachycardia, a narrow, low voltage QRS with alternating amplitudes, no peaked T waves, no QT prolongation, and some minimal ST elevation in II, III, and aVF (without significant reciprocal STD or T wave inversion in aVL). The beat-to-beat variation in QRS amplitude and morphology is electrical alternans.
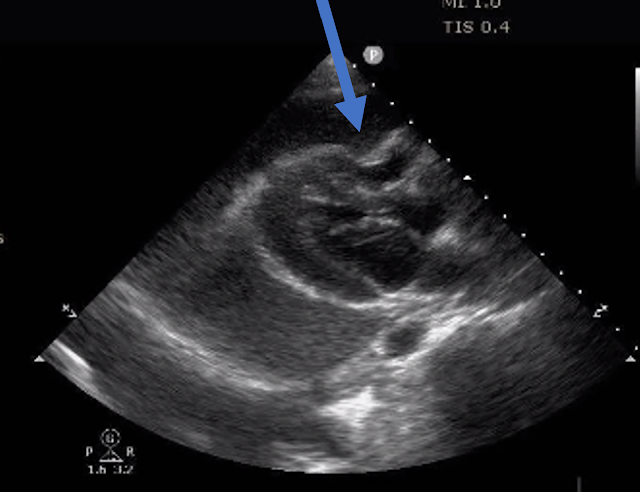
A bedside cardiac ultrasound was performed with a parasternal long axis view demonstrated below:
There is a large pericardial effusion with collapse of the right ventricle during systole. It is difficult to tell if there is collapse during diastole due to the patient’s tachycardia. However, if you freeze the ultrasound clip and scroll forwards and backwards to find a time during the clip where the patient’s mitral valve is open, you know the heart is filling, and is therefore in diastole.
This photo shows the heart in diastole and at the arrow you can see caving in of the right ventricle. Some say this looks like someone jumping on a trampoline. Diastolic collapse of the right ventricle is one of the defining features of cardiac tamponade. To diagnose pericardial tamponade, you need to have a pericardial effusion (the size of the effusion doesn’t necessarily matter) + right atrial diastolic collapse OR right ventricular diastolic collapse. Right atrial diastolic collapse is the earliest sign, but the patient needs to have right atrial collapse for at least 1/3 of the cardiac cycle which can be difficult to identify with ultrasound. So, we usually diagnose tamponade with right ventricular diastolic collapse.
This patient’s pericardial effusion may likely be subacute given the size and echogenicity of the effusion (new blood is anechoic and this looks more isoechoic).
Given her tachycardia and episodes of syncope, the patient was judged to be in compensated obstructive shock with very high risk of imminent decompensation. Cardiology emergently came down to see the patient and took her immediately to the cath lab for a pericardiocentesis (if the cardiologist and cath lab had not been immediately available, then the EM team would have needed to perform pericardiocentesis). A pericardiocentesis was performed by the subxiphoid approach with fluoroscopy. 780 cc of bloody fluid was removed from the pericardial cavity. For reference, a normal heart has about 25-50 cc in the pericardial space. Fluid samples were sent for culture and cytology and results showed malignant cells. A repeat POCUS showed resolution of her pericardial effusion. She was discharged after a short hospitalization with oncology and cardiology follow-up.
As emergency physicians, we see various etiologies of pericardial effusions. The table below shows common causes of tamponade in medical patients. Approximately 40% of tamponade cases in medical patients are due to metastatic malignancy. The second most common cause of medical cardiac tamponade is acute idiopathic pericarditis. Less common etiologies include uremia, bacterial or tubercular pericarditis, chronic idiopathic pericarditis, hemorrhage, and other causes such as autoimmune diseases, radiation, myxedema, etc.
The classic presentation of pericardial tamponade is Beck’s Triad which is hypotension, JVD, and muffled heart sounds. Pericardial tamponade is also associated with pulsus paradoxus which is an abnormally large drop in systolic blood pressure greater than 10 mmHg during inspiration. Beck’s triad only happens all 3 together in approximately 1/3rd of patients. This patient was reported to have distant heart sounds but was not hypotensive and did not have JVD according to documentation.
Smith comment: First, IV fluids are indicated to improve preload. Even in tamponade, one can improve RV output and LV filling with an IV fluid bolus -- it increases filling pressures and thus filling volumes. At our hospital, I think all of our docs would want to place a pigtail catheter in the ED, under ultrasound guidance and not wait for cardiology to take the patient to the cath lab. This patient is only pseudo-stable. She has already had syncope. Her pulse is 125. See how unstable these patients can be by reading this: A young woman in her early 20s with syncope
My colleague, Denise Fraga MD, summarizes the sonographic features of cardiac tamponade:
Sonographic tamponade features
References:
Klein AL, Abbara S, Agler DA, Appleton CP, Asher CR, Hoit B, Hung J, Garcia MJ, Kronzon I, Oh JK, Rodriguez ER, Schaff HV, Schoenhagen P, Tan CD, White RD. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013 Sep;26(9):965-1012.e15. doi: 10.1016/j.echo.2013.06.023. PMID: 23998693.
Appleton
C, Gillam L, Koulogiannis K. Cardiac Tamponade. Cardiol Clin. 2017
Nov;35(4):525-537. doi: 10.1016/j.ccl.2017.07.006. PMID: 29025544.
Learning Points
Echocardiographically, pericardial tamponade features a pericardial effusion + right ventricular diastolic collapse.
The beat-to-beat variation in the QRS complexes (electrical alternans) is a classic ECG finding of a large pericardial effusion or pericardial tamponade.
- For clarity in Figure-1 — I've reproduced her initial ECG.
-USE.png) |
| Figure-1: The initial ECG in today's case. |
- This is not a bigeminal rhythm in the usual sense — because both the PR interval and R-R interval remain constant throughout the tracing. There are no premature beats. Instead (as per Drs. Meyers and Folk) — this is electrical alternans!
- Note that the frontal plane axis shifts with each beat (ie, from being isoelectric in lead I — to being markedly negative in this lead).
- In lead V1 — every-other-beat shows a tiny QRS with an incomplete RBBB pattern.
- Overall QRS amplitude is markedly reduced — especially every-other-beat. Thus, there is diffuse low voltage.
- There appears to be some ST elevation in leads II and aVF, as well as to a lesser extent in the lateral chest leads.
- IMPRESSION: The overall appearance of this ECG is not suggestive of either acute PE or an acute cardiac event. Instead — the KEY for determining the etiology of ECG findings in Figure-1 rests with the history and the diagnostic Echo (that confirms a large pericardial effusion).
- The above said — The history in today's case, in association with the dramatic appearance of electrical alternans (with beat-to-beat shift in the baseline over the course of the long lead rhythm strip in Figure-1) — immediately points to a large pericardial effusion as the most likely cause.
Figure-2: Causes of Low Voltage on ECG (Figure reproduced from My Comment at the bottom of the page in the November 12, 2020 post in Dr. Smith's ECG Blog).
- Electrical alternans is a general term that encompasses a number of different pathophysiologic mechanisms. Its occurrence is not limited to pericardial tamponade — but instead has been associated with an expanding array of clinical conditions.
- Distinction should be made between electrical and mechanical alternans. The term "alternans" itself — merely indicates that there is phasic fluctuation in some cardiac signal from one beat to the next within the cardiac cycle. This may be in the strength of the pulse (or the blood pressure recorded) — or it may be in one or more waveforms in the ECG recording.
- Pulsus alternans — is a mechanical form of alternans. The rhythm is regular — but cardiac output varies from beat-to-beat. It is seen with severe systolic dysfunction. Pulsus alternans should be distinguished from a bigeminal pulse — in which a weaker beat follows the stronger beat by a shorter time interval (as occurs when the alternating beat is a PVC, which understandably generates less cardiac output).
- Pulsus alternans should also be distinguished from pulsus paradoxus — in which there is a palpable decrease in pulse amplitude (or a measured drop of >10 mm in blood pressure) during quiet inspiration. While pulsus alternans and paradoxus may both be seen with pericardial tamponade — they are different phenomena than the various types of electrical alternans.
- That said — Did YOU also See the much more subtle beat-to-beat variation in R wave amplitude in the long lead II rhythm strip in Figure-3?
- While not definitive (See below) — the finding of electrical alternans in an SVT rhythm strongly suggests reentry as the mechanism.
-USE.png) |
| Figure-3: I’ve enclosed within a RED rectangle the 3 leads in this tracing in which there is clear evidence of electrical alternans. (Figure reproduced from My Comment at the bottom of the page in the September 7, 2020 post in Dr. Smith's ECG Blog). |
- Electrical alternans — was first observed in the laboratory by Herring in 1909. It was reported clinically by Sir Thomas Lewis a year later, who characterized the phenomena as occurring, “either when the heart muscle is normal but the heart rate is very fast or when there is serious heart disease and the rate is normal”. This 1910 description by Lewis serves well to this day to remind us of the 2 principal clinical situations in which electrical alternans is most often encountered: i) Supraventricular reentry tachycardias; and ii) Pericardial tamponade.
- Returning to Figure-1: The principal variation that we see in this tracing relates to a repetitive pattern of alternate beat change in QRS morphology. Interval duration does not vary. There may be slight variation in some leads in P wave and ST-T wave morphology — but I thought this to be minimal compared to the much more obvious change in QRS morphology.
- Repolarization Alternans — entails beat-to-beat variation in the ST segment and/or T wave. Alternation in ST segment appearance (or in the amount of ST elevation or depression) — is often linked to ischemia. In contrast — T wave alternation is more often associated with changes in heart rate or in QT duration (especially when the QT is prolonged). In patients with a long QT — T wave alternans may forebode impending Torsades de Pointes. Both ST segment and T wave alternans have been known to precede malignant ventricular arrhythmias. Thus, this type of electrical alternans may convey important adverse prognostic implications when seen in certain situations. That said — a variety of clinical conditions have been associated with repolarization alternans, such that adverse prognostic implications do not always follow. Among these clinical conditions are congenital long QT syndrome — severe electrolyte disturbance (hypocalcemia; hypokalemia; hypomagnesemia) — alcoholic or hypertrophic cardiomyopathy — acute pulmonary embolus — subarachnoid hemorrhage — cardiac arrest and the post-resuscitation period — and various forms of ischemia (spontaneous or induced by treadmill testing or other stimulus).
- Conduction and Refractoriness Alternans — entails variance of impulse propagation along some part of the conduction system. This may result from fluctuations in heart rate or in nervous system activity or from pharmacologic treatment. ECG manifestations from this form of alternans may include alternating appearance of the P wave, QRS complex or alternating difference in P-R or R-R interval duration. In particular — QRS alternans during narrow SVT rhythms has been associated with reentry tachycardias. While identification of QRS alternans during a regular SVT often indicates retrograde conduction over an AP (Accessory Pathway) — this phenomenon has also been seen in patients with simple PSVT/AVNRT that exclusively limits its reentry pathway to the AV Node. Therefore — identification of QRS alternans during a regular SVT does not prove the existence of an accessory pathway. Conduction and refractoriness alternans may be seen with WPW-related as well as AV Nodal-dependent reentry tachycardias — atrial fibrillation — acute pulmonary embolus — myocardial contusion — and severe LV dysfunction. NOTE: On occasion — Alternans may be seen with monomorphic VT (Maury and Metzger).
- Cardiac Motion Alternans — is the result of cardiac movement rather than electrical alternation. The most important clinical entity associated with motion alternans is large pericardial effusion — though motion alternans has also been observed in some cases of hypertrophic cardiomyopathy. It is important to appreciate that not all pericardial effusions produce electrical alternans. Development of total electrical alternans (of P wave, QRS complex and T wave) — is likely to be a harbinger of impending tamponade. Unfortunately — the sensitivity of total electrical alternans is poor for predicting tamponade (ie, most patients who develop tamponade do not manifest preceding electrical alternans). Therefore — it may be helpful if you see total electrical alternans in a patient with a large pericardial effusion — but failure to see this ECG sign in no way rules out the possibility that tamponade is occurring. Echo studies in patients with documented cardiac tamponade confirm that electrical alternans is synchronous with and a direct result of the pendulous movement of the heart within the enlarged, fluid-filled pericardial sac of a patient with large pericardial effusion.
- In practice — It appears that electrical alternans is most often seen in association with regular SVT rhythms (as seen in Figure-3). Seeing it in this context suggests (but does not prove) the existence of an AP (Accessory Pathway). Regardless of whether the mechanism of the regular SVT is AVNRT or AVRT — it is likely that reentry is involved. This conclusion may prove useful in contemplating potential investigative and therapeutic interventions.
- In a patient with pericarditis — OR — a large heart on chest X-ray — OR — simply unexplained dyspnea (as in today's case) — recognition of electrical alternans should suggest the possibility of a significant pericardial effusion that may be associated with tamponade.
- The above said — Electrical alternans is a nonspecific ECG sign that may also indicate myocardial ischemia, LV dysfunction and/or possibility of any of a number of other precipitating factors. BOTTOM Line: If you see electrical alternans — Look for an underlying clinical condition that may be responsible for this ECG sign.
- Development of electrical alternans per se — conveys no adverse prognostic implications beyond those associated with severity of the underlying disorder. Two exceptions to this general rule are: i) In a patient with QT prolongation or severe ischemia — recognition of electrical alternans may portend deterioration to Torsades or VT/VFib; and, ii) In a patient with a large pericardial effusion — development of total electrical alternans (of P wave, QRS complex and T wave) suggests there may now be tamponade.
- FINAL Thought: Keep in mind that not all cases of pericardial effusion will manifest low voltage and electric alternans. The pathophysiology behind electrical alternans with a large pericardial effusion — is a "swinging heart" within the pericardial sac. Thus, alternans is unlikely to be seen with smaller effusions — and even with larger effusions, not all cases manifest alternans.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.