A 40-something male with no previous cardiac disease presented with chest pain.
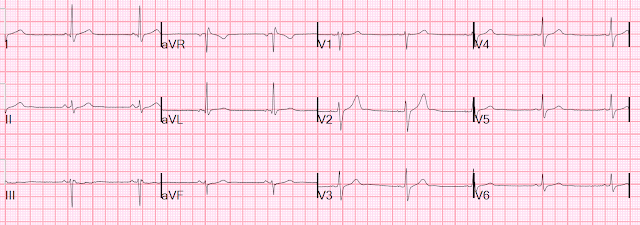
Here is his ECG:
There is no clear evidence of OMI or ischemia. There is a tiny amount of STE in aVL, but it is NOT in the context of a tiny R-wave. There is a tiny amount of STD in lead III, with some non-specific T-wave flattening.The pain continued and the first high sensitivity troponin I returned at 105 ng/L
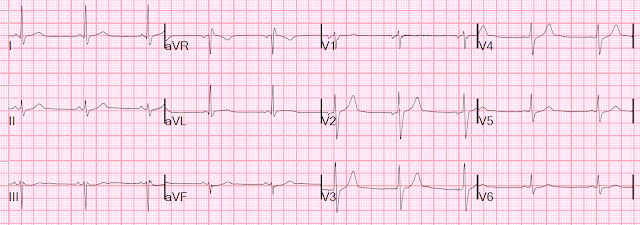
Another ECG was recorded:
At this point, with continued pain, cath lab activation is indicated. Acute chest pain that is persistent (refractory to treatment), with a significantly elevated tropoinin, is due to OMI until proven otherwise. even in the absence of ECG findings.
But the cath lab was not activated.
They waited for a second, 2 hour, troponin, which returned (at 3 hours after patient presentation) at 258 ng/L.
Cath lab was activated.
They recorded a third ECG before intervention:
No significant differenceAngiogram:
Impression and Recommendations:
Culprit for the patient's non-ST elevation myocardial infarction is a thrombotic occlusion of the mid circumflex
Formal Echo
Normal left ventricular cavity size, normal wall thickness and normal LV systolic function.
The estimated left ventricular ejection fraction is 56 %.
Regional wall motion abnormality-anterolateral, hypokinetic to akinetic.
Regional wall motion abnormality-inferolateral, hypokinetic to akinetic.
Regional wall motion abnormality-basal to mid anterior, hypokinetic
Next day ECG after PCI:
There only NOW appears to be some evidence of OMI, but the artery was open. There is "inferior ST depression" which is nearly always reciprocal to high lateral ST elevation, seen or unseen. Here it is seen in I and aVL![]()
- Unfortunately — cath lab activation was delayed in today's case for a full 3 hours.
-USE%20copy.png) |
| Figure-1: I've labeled the 1st, 2nd and 4th tracings in today's case (See text). |
- Small (insignificant) septal Q waves were seen in high-lateral leads I and aVL.
- R wave progression was normal (with transition, where the R wave becomes taller than the S wave is deep — occurring normally between leads V2-to-V4).
- Subtle and nonspecific ST-T segment flattening in several limb leads (ie, leads III, aVL and aVF).
- I thought the T wave in lead V2 was taller and more peaked than-it-should-be given R wave amplitude in this lead (ie, the T wave is clearly taller than the R wave in V2).
- T waves in each of the chest leads were positive — and the T wave in lead V1 is clearly taller than the T wave in lead V6 (Compare T wave amplitudes in these 2 leads within the BLUE squares in ECG #1).
PEARL: When T waves in each of the chest leads are upright (as they are in ECG #1) — the T wave in lead V1 is usually not taller than the T wave in lead V6. This "imbalance of precordial T waves" is not seen very often — and in the “right” clinical setting, has been associated with recent OMI from a LCx culprit artery (See Manno et al: JACC 1:1213, 1983 — and the July 17, 2013 post by Salim Rezaie in ALiEM).
- NOTE: This is not to say that tall, upright T waves in lead V1 might not sometimes be the result of a repolarization variant or a mirror-image reflection of LV “stain” that can sometimes be seen in anterior leads. Instead — it is simply to say that on occasion — I have found recognition of a tall, upright T wave in lead V1 that is clearly taller than the T wave in lead V6 to be a tip-off to an acute coronary syndrome that I might not otherwise have recognized (For 2 more examples of this finding — See My Comments at the bottom of the page in the October 23, 2020 post — and in the March 26, 2022 post of Dr. Smith's Blog).
- To Emphasize: As isolated findings — I probably would not think much of the T wave in lead V2 of ECG #1 (which by itself in a less symptomatic patient, could be a normal variant) — nor would I think much of an upright T wave in lead V1. BUT — in the clinical setting of this patient presenting to the ED for severe new chest pain with: i) A T wave in lead V2 that looks like it could be hyperacute — and ii) The "imbalance" of precordial T waves (T in V1>V6) — and iii) The nonspecific but-nevertheless-real ST-T wave flattening in leads III, aVL, aVF — my index of suspicion for an acute evolving event was raised.
- As per Dr. Smith — the significantly elevated initial troponin value — in association with severe, new chest pain refractory to treatment should have been enough to indicate prompt cath (even if the above ECG findings would not have been present).
- Given concern from ECG #1 that the T wave in lead V2 might be hyperacute — I thought there was a definite increase in T wave peaking and T wave amplitude in leads V3 and V4 of ECG #2 (within the RED rectangles of this 2nd tracing).
- NOTE: These changes are subtle. The challenge in assessing serial tracings is having to evaluate the significance (if any) when changes are slight — and when such changes are potentially countered by a shift in frontal plane axis, chest lead electrode placement and/or a worsening of ST-T wave changes in some leads but improvement in others. So although T wave amplitude in leads V1,V2 was less in ECG #2 — I thought the presence of potentially 3 successive leads (V1,V2,V3) with hyperacute T waves in ECG #2 more than made up for this — especially given what now clearly looks like reciprocal ST changes in lead aVF. In a patient with refractory new chest pain — I interpreted my comparison of ECGs #1 and #2 as suggestive of dynamic ST-T wave change.
- Additional support that this ST elevation is real — is forthcoming from mirror-image-opposite curved ST depression (reciprocal change) in lead III. Reciprocal changes in the other 2 inferior leads (leads II and aVF) were also clearly increased compared to the initial tracing (ECG #1).
- A final finding consistent with posterior infarction — is the increase in relative R wave (compared-to-S-wave) amplitude in leads V1 and V2 of ECG #4. In comparison — the S wave was predominant in both leads V1 and V2 of ECG #1.



No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.