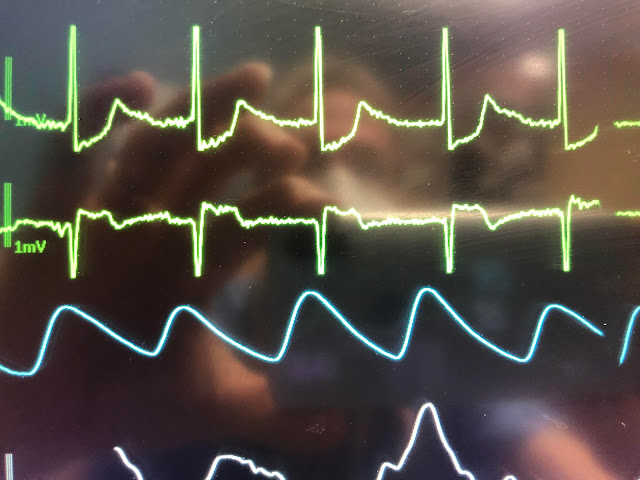
The lower is analogous to V1
What do you think?
The ST depression here is about 30% of the height of the R-wave. The ST Elevation is about 30% of the depth of the S-wave
I wanted to show the residents how poorly this correlates with a 12-lead ECG, so we recorded one at the same time:
The STE in V1 is less than 10% of the S-wave
The STD in V5 is a bit difficult to measure due to artifact, but let's say that it is 3 mm, in the context of a 32 mm R-wave, or about 10%
This patient's ST abnormalities are baseline due to Digoxin effect.
The lesson to be learned is that the monitor often greatly exaggerates STE and STD. It has to do with electronic filtering, and a lot of engineering that I don't really understand.
But Christopher Watford understands it very well, and so I am having Christopher explain it:
The explanation has to do with "high pass filtering of the 'frequencies'". This is NOT the sampling frequency (for instance, a 12-lead ECG measures the voltage 500x per second (500 Hz) which is the sampling frequency.
This is a different kind of frequency:
From Christopher:
"Frequency is a property of a signal you record. The ECG
is a very complicated signal. We can decompose a complicated signal into
many simple signals (sine waves). Each simple signal has a frequency,
amplitude, and phase. This is a rough definition of Fourier Analysis.
"Filtering
on frequency can be thought of as subtraction of these simple signals
based on a rule: their frequency. The monitor then displays for you the
"sum" of the remaining signals.
"Pretend
an ECG is an equation like: 2x + 5y + z, and that x, y, and z are the
frequencies. Now pretend your high pass filter subtracted 2x from your
ECG. You would be left with 5y + z. That's what you'd see.
"Considering
that very rough example, you would say that the filter was _useful_ if
that subtraction removed only the undesirable parts of the signal. But
what if out of 2x, 1.5x was your ST segment?
"Or
what if the filter didn't just subtract 2x but also multiplied the
whole equation by 0.9 and added 0.25x? That's closer to the reality of
real time filtering. You're introducing some distortion because of the
imperfect math."
"As far as filtering and the ECG, it is basically that the more
filtering you use the more distortion you see. Four types of filters are
found on cardiac monitors: high pass filters to remove low frequency
artifacts, low pass filters to remove high frequency artifacts, notch
filters to remove a specific frequency such as your A/C power, and
common mode rejection via RL lead to handle D/C interference.
"The
ideal filter for a cardiac monitor is one that preserves the components
you care about and rejects the artifacts you do not care about.
"Our
ST segments are low frequency signals, just like baseline wander.
Muscle and movement artifacts are typically high frequency. Everything
else tends to fall in-between (P, QRS, T). So by carving out frequency
within about 0.5-40hz we can have a really good look at the cardiac rhythm as all of the important components fall within that range, and all of the artifacts we don't want fall outside the range.
"The common frequencies of the important components on the ECG:
- Heart rate: 0.67 – 5 Hz (i.e. 40 – 300 bpm)
- P-wave: 0.67 – 5 Hz
- QRS: 10 – 50 Hz
- T-wave: 1 – 7 Hz
- High frequency potentials: 100 – 500 Hz
"The common frequencies of the artifact and noise on the ECG:
- Muscle: 5 – 50 Hz
- Respiratory: 0.12 – 0.5 Hz (e.g. 8 – 30 bpm)
- External electrical: 50 or 60 Hz (A/C mains or line frequency)
- Other electrical: typically >10 Hz (muscle stimulators, strong magnetic fields, pacemakers with impedance monitoring)
"The interesting bit is what happens to the frequencies we filter out in real time.
Filtering generally works on the principle of decomposing a wave into
its constituent parts (Fourier Analysis). You can think of the ECG as
the sum of a bunch of "common" waves of various frequencies, amplitudes,
and phases. Low pass filters which reject high frequency artifacts tend
to attenuate the amplitude of an ECG.
High pass filters, however, instead tend to introduce a phase shift.
Worse still, this phase shift can occur in a band around the filter
(i.e. it affects the contiguous harmonics). This band of frequencies
affected is relatively large and impacts the ST segments in a noticeable
manner. Real time ECG filtering is where you see this, as there exist
post-processing techniques for 12-lead ECGs that do not exhibit these
limitations.
If muscle artifacts and the
QRS land in the same frequency range, you may wonder why we do not see
such distortion. The QRS has a much higher amplitude to begin with
compared to muscle artifact, allowing it to tolerate far more
attenuation before you lose the meaningful components of that signal. In
contrast, ST-segments are rarely high amplitude and thus will be
affected quite easily by filtering.
I
simulated applying a 1 Hz high pass filter to an ECG lead using GNU
Octave, and the distortion to the ST segments is quite pronounced:
Compare that same ECG with a 0.05 Hz high pass filter, as you would
find on a 12-Lead ECG, and the distortion to the ST segments are
minimal (<0.1 mV):
.png)
Putting the graphs aside, you simply pick the filters that match
the frequency range you care about. Monitors are for monitoring rhythm
and 12-Leads are for detailed monitoring of electrical activity. And
even then, you need to know your device. Many EMS monitors record
12-Leads at 0.05-40Hz to keep a cleaner tracing. If you're looking for
epsilon waves or subtle J-waves, a 40Hz low pass filter is much too
aggressive. You likely need 100 or even 150 Hz!
Many
devices these days have special functions to address this problem. Some
have special filtering modes to track ST-segments and others allow you
to change the monitoring frequencies as needed. So, I'm not saying you
can't spot acute ST-elevation on a cardiac monitor, but you don't know
what's been left out! It is very hard to look at a filtered ECG and
guess what changed or is missing, perhaps a fun party trick but not
something I'd bet on without a 12-Lead.
===================================
Comment by KEN GRAUER, MD (4/20/2019):
===================================
It is good to periodically show clinical examples of how misleading ST segment deviation on an ECG monitor can be. As worrisome as the ST depression in lead V5 (and the ST elevation in lead V1) of the above monitoring strip is — Dr. Smith showed that it is not real!
While far from expert in this area — I reviewed the essentials of Filter Settings in My Comment at the bottom of the page in the March 4, 2019 post in Dr. Smith's ECG Blog. Dr. Smith conveys "the Short Answer" above — which for clarity I repeat here: - ST segment deviations (elevation or depression) are not reliably conveyed on an ECG monitor. They may or may not be "real".
- If ever you see something of potential concern on a monitor (ie, significant ST elevation or depression) — then immediately obtain a complete 12-lead ECG. Doing so is the only way to know whether or not there is true ST segment deviation.
- The chance that an abnormal appearance of the ST-T wave on monitoring reflects acute ischemia or infarction is greater IF — you have been monitoring a patient over time, and without any change in lead placement, you all-of-a-sudden note a difference in ST-T wave appearance.
- Regardless of whether or not there has been ongoing monitoring — the only way to know if the ST segment deviation you see is "real" — is to immediately obtain a 12-lead ECG.
- For the "Longer Answer" — Christopher Watford's SUPERB discussion (above) serves as a mini-course syllabus on the subject! I will frequently refer back to the excellent guidelines he provides.
- For a user-friendly "Intermediate Answer" — Please check out My Comment in the March 4, 2019 post in Dr. Smith's Blog.


.png)
.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.