A young man had an accidental exposure to carbon monoxide (CO). He was comatose and intubated and his initial Carboxyhemoglobin level was over 50%.
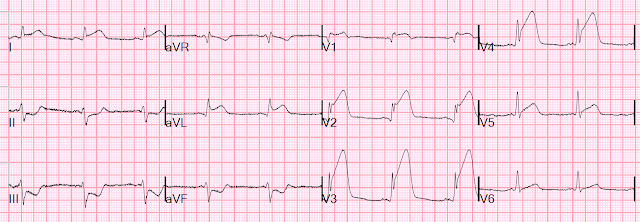
An ECG is always recorded for CO toxicity. This was his ECG.
My interpretation was that this was all normal variant ST Elevation.
Inferior STE: there are prominent J-waves in all leads. There is no reciprocal ST depression in aVL.
Anterior STE: Prominent J waves and high QRS amplitudes.
If we use the LAD-normal variant formula, we get:
QTc = 436 ms
R-wave V4 = 13 mm, QRS V2 = 21 mm, STE at 60 ms after J pt in V3 = 2.5
Formula value = 18.7. This is suggestive of LAD occlusion. However, the variable which most contributes to this is the QTc of 436 ms, which is quite long and skews the result of the formula to LAD occlusion. For comparison, if the QT were an average of that of LAD occlusion (420 ms) vs. Normal variant (390 ms) from our study, the QTc would be 405 ms and the formula value would be 17.06, which is rarely seen in LAD occlusion
What we have evidence for, but is not widely known, is that CO Toxicity likely lengthens the QT interval. So this relatively long QT interval is NOT due to ischemia but may be a result of CO Toxicity. Yelken B et al. The assessment of QT intervals in acute carbon monoxide poisoning
I was not worried about this ECG.
The coma completely recovered with 3 hyperbaric oxygen treatments in our world class state-of-the-art-facility. https://hennepinem.com/fellowships/hyperbaric-medicine/.
Read more about CO poisoning and cardiac ischemia here (ECG is pasted below): What is the treatment for this subendocardial ischemia?
Troponin peaked at 43 ng/L (barely elevated; most patients with CO toxicity this severe have significantly elevated troponin simply from the oxygen deprivation AND from directly toxicity of CO on myocardial cells)
Here is the next day ECG:
CO poisoning. Routine ECG recorded before hyperbaric therapy....Are they related?
With this ECG:
________________________
See this typical case of cO poisoning:
What is the treatment for this subendocardial ischemia?
===================================
MY Comment, by KEN GRAUER, MD (2/18/2022):
===================================
- The KEY to accurate comparison of serial tracings — is to be sure you are “comparing apples with apples — instead of comparing apples with oranges”.
- It is common to see changes in frontal plane axis and/or in chest lead R wave progression on serial tracings. This may be due to slight changes in the incline of the patient’s bed (ie, if on the initial tracing the patient was too dyspneic to lie flat) — or, to changes in chest lead electrode placement — or, simply due to the difficult-to-account-for slight variation in QRST morphology that sometimes occurs from one tracing to the next. These changes may produce differences in QRS and ST-T wave morphology from one tracing to the next not due to any change in the patient’s clinical condition.
- Is the frontal plane Axis the same in both tracings?
- Is R Wave Progression (and the area of Transition) the same?
- IF either the Axis or R Wave Progression changed — How did this change affect QRS and ST-T wave appearance?
ANSWER:
- Since there has not been any change (other than minimal increase in T wave amplitude in lead aVL of ECG #2) — we can confidently say "No change".
- The area of Transition (where height of the R wave becomes taller than the S wave is deep) — had been between leads V3-to-V4 in ECG #1. Note that R wave amplitude equaled S wave depth already in lead V3 in ECG #1.
- Transition occurs later in ECG #2 (ie, R wave height does not exceed S wave depth until leads V4-to-V5 — and the QRS was still predominantly negative in lead V4).
- This means that serial comparison looking for ST-T wave changes in Figure-1 between these 2 tracings is not like "comparing apples with apples" — because transition is delayed in ECG #2, and QRS morphology is not the same.
- Isn't the T wave in lead V1 of ECG #2 now negative — whereas it was positive in ECG #1?
- Isn't the T wave in lead V2 of ECG #1 significantly taller than the T wave in lead V2 of ECG #2?
- Isn't there more J-point ST elevation in leads V2 and V3 in ECG #1?
- I completely agree with Dr. Smith's assessment — that in today's case, the differences we see in ST-T wave morphology between the 2 tracings is unlikely to be clinically significant (and is most likely the result of slight change in chest lead electrode placement).
- Take-Home POINT: Remember to take into account frontal plane Axis and R Wave Progression when comparing serial tracings!
 |
| Figure-1: Comparison of the initial ECG in the ED ( = ECG #1) — with the follow-up ECG done the next day ( = ECG #2). |
The Important Clinical Point:
- T-QRS-D — is defined as the absence of both a J-wave and an S-wave in either lead V2 or lead V3 (and sometimes lead V4). Although simple to define — it’s taken me a bit of practice to become comfortable and confident in its recognition.
- START WITH THIS ONE = step-by-step discussion by Brooks Walsh & Steve Smith about T-QRS-D.
- MORE PRACTICE = 4 examples (3 positive; 1 not for T-QRS-D).
 |
| Figure-2: Comparison between ST elevation in lead V3 due to a repolarization variant (TOP — from the 4/27/2019 post) — vs acute OMI (BOTTOM — from the 9/20/2015 post), which manifests T-QRS-D (See text). |
- ECG #1 ( = TOP tracing in Figure-3): As per Dr. Smith — the ST-T wave changes in this tracing strongly suggest a repolarization variant. In addition to prominent J-point notching in multiple leads (RED arrows in Figure-3) — there is normal R wave progression with ample QRS amplitude — no reciprocal ST depression — similar ST-T wave morphology in multiple leads (ie, lack of the localizing changes that are typically seen with acute infarction) — and, terminal QRS "slurring" (PINK arrows), that convey similar clinical implications as the prominent J-point notching. Lack of evolution on the repeat tracing done the next day (ECG #2) supported the conclusion that ECG #1 represents a repolarization variant, and is not indicative of an acute cardiac event.
- ECG #3 ( = BOTTOM tracing in Figure-3) — was added to today's case by Dr. Smith to provide an example in which acute CO poisoning was accompanied by an obvious STEMI (The case discussed in detail in the December 9, 2019 post in Dr. Smith's ECG Blog). Note the BLUE arrows — which highlight obvious T-QRS-D, seen here in the 3 leads with the most ST elevation.
 |
| Figure-3: Comparison of ECG #1 and ECG #3 from today's case to illustrate what is — and what is not T-QRS-D (See text). |




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.