A 90 yo with a history of orthostatic hypotension had a near syncopal event followed by chest pain. Chest pain was resolved upon arrival in the ED.
His previous ECG was normal.
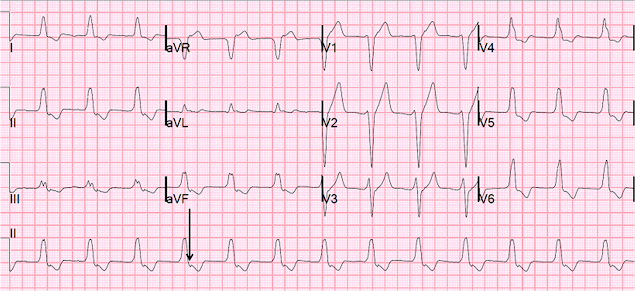
Here is his initial ECG:
Idioventricular rhythm is a common "reperfusion arrhythmia." In other words, after reperfusion therapy for STEMI, the appearance of AIVR is usually a good sign, meaning that the artery is reperfused.
Some would argue that it cannot be "idio" if it conducts to the atria. But by usage, even these are called AIVR. It is very important to not try to treat AIVR. In fact, especially if there is no conduction to the atria, suppression of AIVR may result it asystole. This is a safe rhythm and usually has reasonable cardiac output, as the ventricles have time to fill.
ECG Diagnosis is either:
1) junctional rhythm with new LBBB, and possibly ischemia
2) accelerated idoventricular rhythm with possible ischemia, and possibly related to restoration of normal perfusion.
3) AV nodal re-entry???? with rate-related LBBB. Our electrophysiologist, Rehan Karim, states he has ablated AVNR"T" ("T" because it is not tachycardia) in a 90 year old, and that he has seen rate-related BBB at very slow rates.
A repeat ECG had sinus rhythm at a rate of 54 and normal conduction (no LBBB), and was completely normal with no ischemia. The second explanation (AIVR), whether as a reperfusion dysrhythmia or not, seems most likely. The slow sinus rate supports the notion that this could be rate-related BBB.
The patient had a transient rise in troponin I from 2 values less than 0.012 ng/ml (undetectable) to 0.020 ng/ml (detectable but still below the 99% reference threshold).
Chest pain and possible ischemia were attributed not to ACS, but to transient hypoperfusion from orthostatic hypotension.
So there may have been 1) transient AIVR, or 2) junctional rhythm with transient or rate-related LBBB, or even 3) AVNRT with rate-related LBBB. Exactly how they relate to ischemia, chest pain, and reperfusion can only be speculated about.
His previous ECG was normal.
Here is his initial ECG:
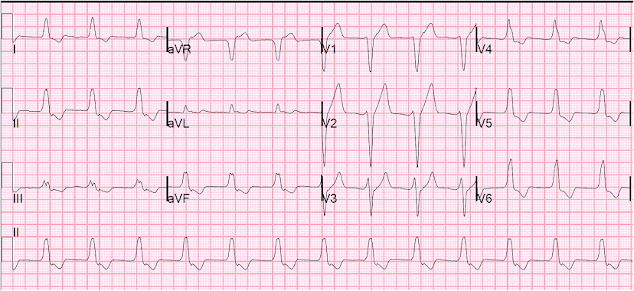 |
| There is a wide complex regular rhythm at a rate of about 80. What is it? Answer below. |
Idioventricular rhythm is a common "reperfusion arrhythmia." In other words, after reperfusion therapy for STEMI, the appearance of AIVR is usually a good sign, meaning that the artery is reperfused.
Some would argue that it cannot be "idio" if it conducts to the atria. But by usage, even these are called AIVR. It is very important to not try to treat AIVR. In fact, especially if there is no conduction to the atria, suppression of AIVR may result it asystole. This is a safe rhythm and usually has reasonable cardiac output, as the ventricles have time to fill.
ECG Diagnosis is either:
1) junctional rhythm with new LBBB, and possibly ischemia
2) accelerated idoventricular rhythm with possible ischemia, and possibly related to restoration of normal perfusion.
3) AV nodal re-entry???? with rate-related LBBB. Our electrophysiologist, Rehan Karim, states he has ablated AVNR"T" ("T" because it is not tachycardia) in a 90 year old, and that he has seen rate-related BBB at very slow rates.
A repeat ECG had sinus rhythm at a rate of 54 and normal conduction (no LBBB), and was completely normal with no ischemia. The second explanation (AIVR), whether as a reperfusion dysrhythmia or not, seems most likely. The slow sinus rate supports the notion that this could be rate-related BBB.
The patient had a transient rise in troponin I from 2 values less than 0.012 ng/ml (undetectable) to 0.020 ng/ml (detectable but still below the 99% reference threshold).
Chest pain and possible ischemia were attributed not to ACS, but to transient hypoperfusion from orthostatic hypotension.
So there may have been 1) transient AIVR, or 2) junctional rhythm with transient or rate-related LBBB, or even 3) AVNRT with rate-related LBBB. Exactly how they relate to ischemia, chest pain, and reperfusion can only be speculated about.

Don’t mean to split hairs here, but I wanted to make a minor point on semantics of terminology. I would drop the prefix "idio" from this interpretation and fully spell out the rhythm as accelerated ventricular rhythm while forgoing the use of any non-standard acronym like AVR since it could be confused with lead aVR. Since there is 1:1 retrograde conduction to the atria, the ectopic ventricular focus has control over the entire heart as a whole. Not just the ventricles, but the atria as well.
ReplyDeleteThe prefix “idio-“ implies that the ventricles have their own pacemaker all to themselves and are beating independently of the atria (from the Greek, idios, which means “one’s own,” “private,” “personal”). (1)
In leads V1 and V2, there are fat, little r-waves that are >0.03s wide. If you measure from the beginning of these r-waves to the nadir of the S-waves, that interval is delayed (i.e., late) at about 0.12s. Any duration >0.07s would strongly favor an ectopic ventricular focus. Dr. Wellens popularized this criteria and Dr. Marriott referred to it as the "Philadelphia clue". (2,3)
Reference/Source:
1.) Marriott HJL. Practical Electrocardiography. 8th ed. Baltimore: Williams & Wilkins, 1988, p. 277, 329, & 373.
2.) Marriott HJL. Marriott’s Manual in Electrocardiography. 1st ed. Naples: Trinity Press, 1999, p. 101
3.) http://heart.bmj.com/content/86/5/579.full
I like your blog... thanks.
ReplyDeleteWhat do you think about ST change in aVr?
Was this meaningful or reciprocal?
Semantically, you are correct. However, in usage (which is usually considered the standard for correct language), AIVR is the name for an accelerated automatic rhythm of the ventricles.
ReplyDeleteHowever, your point is important in that, if the rhtyhm did not conduct to the atria, it would imply AV block. This would make it much more dangerous if, for example, a clinician tried to treat to suppress the ventricle, then there would be no escape for the AV block and it may result in asystole.
This is the normal discordant ST elevation in aVR seen in LBBB morphology.
ReplyDeleteNow that you mention it Dr. Smith, that reminds me I've seen a similar case published in a textbook where the patient converts into atrial flutter from sinus rhythm and subsequently develops AIVR dissociated from the flutter. At this point, the only thing generating a pulse is the AIVR. Consequently, somebody was horrified enough by the appearance of the AIVR to administer a bolus of lidocaine. The ensuing result was ventricular asystole as the AIVR was completely suppressed. The only thing visualized on the baseline was the sawtooth pattern of the flutter waves and no sign of any ventricular activity. Therefore, no cardiac output and no pulse.
ReplyDelete1.) Conover MB. Understanding Electrocardiography. 7th ed. St. Louis: C.V. Mosby, 1996, p. 113 & 116.
what about this ecg? https://dl.dropboxusercontent.com/u/32778364/exact-moment--change-to-LBBB.jpg
ReplyDeleteI can barely see the tracing as it is very blurry, but appears to me to be sinus with LBBB. Am I missing something?
DeleteSteve Smith
The above ECG record looks rather at the rhythm of the atrioventricular junction, carried out with the accompanying left bundle branch block - this is demonstrated by the retrograde P <100 ms wave for the QRS syndrome.
ReplyDeleteThanks for the blog Dr. Smith. A great inspiration to learn ECGs : ) and a favourite now world over.
ReplyDeleteDr. Smith, how do you figure that the P wave is upright in lead II ?? It could be inverted and produce the same curve in lead II if it came a touch earlier, couldn't it ?? Or it could be a markedly long 1st degree heart block since the disturbance in the ST segment has same morphology in I, II, aVF and V4-6 and inverted in aVR ?? Thanks in advance : )
It is not upright. It is inverted because retrograde, with VA conduction.
Delete