For another fascinating related ECG, click here:
Acute MI from LAD occlusion, or early repolarization?
Case:
This is a 46 yo male with acute onset of chest pain, in distress, who called the ambulance. He arrived and had this ECG recorded at 0118 AM.
A followup ECG and the answer is below.
There is 1 mm of ST elevation in V2 and V3, so this meets the criteria for reperfusion by the ACC/AHA guidelines. Unfortunately, the majority of patients who meet such "criteria" do not have MI. The most common reason for ST elevation is early repolarization.
(In this case, the limb leads are suggestive of ischemia as well, with some subtle ST depression inferiorly, suggesting pending ST elevation in aVL due to lateral MI from proximal LAD occlusion.)
I have developed a decision rule to differentiate Anterior STEMI from BER in patients who present to the ED with chest pain. These rules only apply when the DDx is Anterior MI vs. BER. A simple rule is the R-wave rule, which depends on the fact that, in BER, the R-wave is always well developed:
If the mean R-wave amplitude from V2-V4 is less than 5 mm, then it is almost certainly MI. If greater than 5 mm, it is probably BER. A cutoff of 5 mm gives a sensitivity for MI of about 70%, but a specificity of greater than 95%.
There are a couple other more complex rules, one of which uses QTc-B, R-wave amplitude in lead V4, and ST elevation at 60 ms after the J-point in lead V3.
Another equally accurate one, also derived using logistic regression, uses QTc and 2 averages: mean ST elevation at the J point (STEJ) from V2-V4 and mean R-wave amplitude from V2-V4.
Both rely on the findings that the mean ST elevation was higher in the MI group, and the mean QTc in BER is shorter (mean = 390 ms), and mean R-wave amplitude is lower.
If the formula: (1.553 x mean STEJ in mm) + (.0546 x QTc in ms) - (0.3813 x mean RA in mm, not mV) is > 21, vs. less than or equal to 21, then it represents MI with high sensitivity and specificity.
In this case, the values are (1.553 x 1.0) + (.0546 x 420) - (.3813 x 1.17) = 1.553 + 22.93 - 0.3813 = 24.1
Thus, the rule predicts that this is anterior MI.
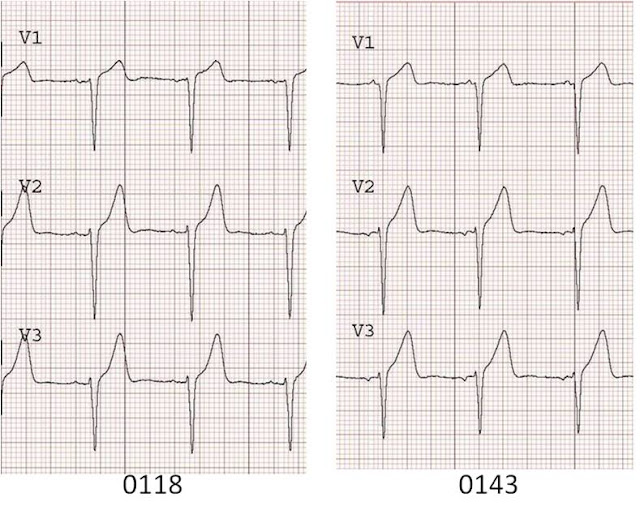
The clinicians were suspicious of MI, so they were smart to obtain serial ECGs. They obtained the second ECG at 0143:
This shows unequivocal straightening of the ST segments, compared to the first ECG. This ST straightening results in T waves which are fattened and "hyperacute". This is diagnostic of anterior STEMI.
In case you can't see this difference in the straightening of the ST segment, here they are side-by-side:
He had a 100% proximal thrombotic LAD occlusion with TIMI-0 flow. It was opened and stented.
The followup ECG might give an idea of what this patient's T-waves looked like before his occlusion:
Acute MI from LAD occlusion, or early repolarization?
Case:
This is a 46 yo male with acute onset of chest pain, in distress, who called the ambulance. He arrived and had this ECG recorded at 0118 AM.
A followup ECG and the answer is below.
There is 1 mm of ST elevation in V2 and V3, so this meets the criteria for reperfusion by the ACC/AHA guidelines. Unfortunately, the majority of patients who meet such "criteria" do not have MI. The most common reason for ST elevation is early repolarization.
(In this case, the limb leads are suggestive of ischemia as well, with some subtle ST depression inferiorly, suggesting pending ST elevation in aVL due to lateral MI from proximal LAD occlusion.)
I have developed a decision rule to differentiate Anterior STEMI from BER in patients who present to the ED with chest pain. These rules only apply when the DDx is Anterior MI vs. BER. A simple rule is the R-wave rule, which depends on the fact that, in BER, the R-wave is always well developed:
If the mean R-wave amplitude from V2-V4 is less than 5 mm, then it is almost certainly MI. If greater than 5 mm, it is probably BER. A cutoff of 5 mm gives a sensitivity for MI of about 70%, but a specificity of greater than 95%.
There are a couple other more complex rules, one of which uses QTc-B, R-wave amplitude in lead V4, and ST elevation at 60 ms after the J-point in lead V3.
Another equally accurate one, also derived using logistic regression, uses QTc and 2 averages: mean ST elevation at the J point (STEJ) from V2-V4 and mean R-wave amplitude from V2-V4.
Both rely on the findings that the mean ST elevation was higher in the MI group, and the mean QTc in BER is shorter (mean = 390 ms), and mean R-wave amplitude is lower.
If the formula: (1.553 x mean STEJ in mm) + (.0546 x QTc in ms) - (0.3813 x mean RA in mm, not mV) is > 21, vs. less than or equal to 21, then it represents MI with high sensitivity and specificity.
In this case, the values are (1.553 x 1.0) + (.0546 x 420) - (.3813 x 1.17) = 1.553 + 22.93 - 0.3813 = 24.1
Thus, the rule predicts that this is anterior MI.
The clinicians were suspicious of MI, so they were smart to obtain serial ECGs. They obtained the second ECG at 0143:
This shows unequivocal straightening of the ST segments, compared to the first ECG. This ST straightening results in T waves which are fattened and "hyperacute". This is diagnostic of anterior STEMI.
In case you can't see this difference in the straightening of the ST segment, here they are side-by-side:
The followup ECG might give an idea of what this patient's T-waves looked like before his occlusion:




Dr. Smith -
ReplyDeleteYou wrote:
"If the mean R-wave amplitude from V2-V4 is less than 5 mm, then it is highly unlikely to be BER. If greater than 5 mm, it is probably MI. A cutoff of 5 mm gives a sensitivity for MI of about 70%, but a specificity of greater than 95%."
Is this a typo?
If the R-wave amplitude is greater than 5 mm, then it's probably MI? Or did you mean to say that it's probably BER?
I have two cases of anterior STEMI vs. BER, and in both cases, it turned out to be anterior STEMI.
In the first case, the mean R-wave amplitude in V2-V4 is less than 5 mm.
In the second case, the mean R-wave amplitude in V2-V4 is greater than 5 mm.
Would it be safe to say that the second case shows anterior STEMI in the presence of BER?
Thanks for another great teaching point!
Tom
Tom,
ReplyDeleteThanks for pointing out the typo. I have corrected it.
Your case with good R wave amplitude is a very interesting one, and points out that neither decision rule is perfect (and the senstivities and specifities were not perfect in the study, either).
Fortunatel for your patient, the diagnosis of STEMI is clear from ST elevation in aVL, with reciprocal ST depression in inferior leads.
But the anterior leads sure do look like early repol, and even have the characteristic J wave!
Thanks,
Steve Smith
Excellent example. I've never heard of the method you described. You didn't mention the use of the R/S ratio to r/o early repol. Is this something that you advocate?
ReplyDeleteI've been following your blog for a while and have yet to comment, so I figured I would. Great blog by the way.
I'm not sure if you have visited my blog yet, but would like to extend an offer. I have a multi-authored blog including Tom B, Rogue medic, and others. It is an educational blog for all emergency practitioners; at this time mostly aimed towards the prehospital clinician. I am always looking for more authors, especially one with your expertise. If you are interested shoot me an email, athompson@leegov.com.
wow that was a great post, glad i pciked the STEMI but still dont have my head around the BER thing...back to the books :P
ReplyDeleteHi Dr. Smith,
ReplyDeleteI find your blog very interesting and informative! I'm Hua, the director of Wellsphere's HealthBlogger Network, a network of over 2,000 of the best health writers on the web (including doctors, nurses, healthy living professionals, and expert patients). I think your blog would be a great addition to the Network and with in our Life as a Doc community, and I'd like to invite you to learn more about it and apply to join at http://www.wellsphere.com/health-blogger. Once approved by our Chief Medical Officer, your posts will be republished on Wellsphere where they will be available to over 5 million monthly visitors who come to the site looking for health information and support. There’s no cost and no extra work for you! The HealthBlogger page (http://www.wellsphere.com/health-blogger) provides details about participation, but if you have any questions please feel free to email me at hua@wellsphere.com.
Best,
Hua
Hi!
ReplyDeleteI have been applying the more complex rule mentioned above to the prehospital ECG of a patient we admitted last week.
Mean STEJ = (2+1+1)/3 = 1.33mm
QTc 392
Mean R-amplitude 0.9mV (9mm)
This gave a score of (1.553 x 1.33) + (.0546 x 392) - (.3813 x 0.9) = 2.06 + 21.4 - 0.343 = 23.12 - which would indicate AMI
The patient received prehospital thrombolysis. However all three troponin measurements were negative... The ECG changes were static over time, and are thought to represent BER.
The post states that the mean QTc in BER is 390, which would alone give a score of 21.29. And as the mean R amplitude is multiplied with a very small factor (0.3813) even larger R amplitudes would deduct very little from this score.
Or is there some problem with the units? Should the mean RA be in mm rather than mV?
Sincerely, Tor Pedersen (EMT and, now also, medical intern)
the rule is almost 90% sensitive and 90% specific when comparing subtle MI to BER. This was true in both a derivation group and validation group. But it's not perfect. Your very small R-wave amplitude (mean of 0.9 mm?!!) is very unusual for BER and is the reason for the false positive.
ReplyDeleteAnd now I see the reason for the misunderstanding. It is mm, not mV!! I should have clarified that. Sorry.
In my series of BER, only 5% had a mean R-wave V2-V4 less than 5mm. And probably none had a mean of 0.9mm, not mV!!
Dr. Smith,
ReplyDeleteBesides the STD and junctional rhythm, there was also a pathological Q-wave in lead III on the first that is not present anywhere else. Is this due to misplacement? Also is a prolonged QTc sensitive for Anterior MI vs. BER? And one last question, I noticed that after reperfusion the R-wave progression is still poor. How long does it take usually until the R-wave progression becomes intact again?
Troy, very good points. It may be lead misplacement. The QRS axis on the first 2 ECGs is about 15 and then 90 on the last. Not sure how to figure which leads were misplaced. On the other hand, acute MI can alter the axis. The QTc is more prolonged in anterior STEMI than in BER, but by itself does not lead to a good cutoff value.
ReplyDeleteRecovery of R-waves is very variable. There may have always been poor progression in this patient, even before LAD occlusion. The point is just as much that early repol always has good R-wave progression as that in MI R-wave progression may be lost.
HI Dr smith. Your blog is very useful. Thanks.
ReplyDeleteI've spotted another small typo.
"Both rely on the findings that the mean ST elevation was higher in the MI group, and the mean QTc in BER is shorter (mean = 390 ms), and mean R-wave amplitude is greater." The mean R-wave amplitude should be smaller not greater.
Thanks! I fixed it.
DeleteOops sorry. I didn't read the sentence properly. You had it right in the first place but the whole sentence is a little odd and confusing. You talk about bot the MI group and the BER group in the same sentence.
ReplyDeleteNo!! YOU had it right. Because of you, I edited the post! Thanks!!
DeleteHi.
ReplyDeleteIn last ECG; there is PRWP which will probably become this patient's baseline. If this patient were to develope chest pain and the initial ECG shows this ecg(last) wouldn't that give false positive AMI?