Written by Pendell Meyers
A man in his 60s called EMS for sudden chest pain and shortness of breath. He was found in moderate respiratory distress, hypertensive, diaphoretic, and hypoxemic. He was given aspirin, nitroglycerin, and placed on noninvasive positive pressure ventilation during transport. Medics recorded a 12-lead and transmitted it to the provider, asking if they wanted to activate the cath lab.
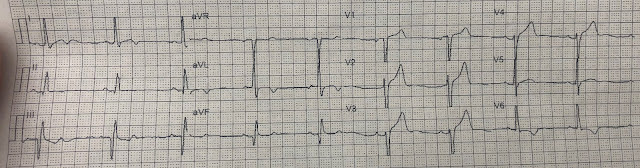
Here is the ECG:
 |
| What do you think? |
Sinus rhythm. In this EMS ECG, as is true for many EMS ECGs, the machine cuts off the S wave voltage at 10 mm. You can see this visually by the subtle but noticeable squared-off waveform of the S wave in leads V2-V3.
In lead aVL, you can see that the machine does not limit the R waves to 10 mm. So as far as I can tell, this machine only limits negative QRS voltage to 10 mm.
In limiting the S wave to 10 mm, this feature of the EMS 12-lead ECG significantly changes the visual proportionality of the ST segments and T waves in the affected leads. If this QRS were only 10 mm or less in amplitude, then these STEs and relatively large T waves in leads V1-V4 could be worrisome for anterior OMI.
But after falling for this trick once, you probably will not make this mistake again. You will see easily that this QRS shows significant voltage and morphology of LVH.
So the provider said no, no prehospital cath lab activation for now and we will evaluate the patient immediately on arrival.
The patient arrived and was already much improved from the paramedics' treatments thus far.
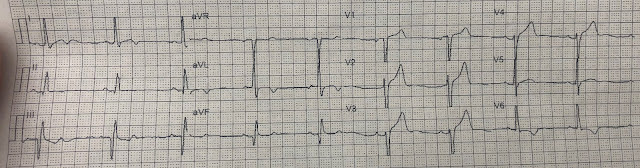
Here was his ED ECG on arrival:
Seeing the full QRS makes all the difference here. With the full QRS complexes available, you can see that it is diagnostic of LVH, with very reasonable and proportionally normal STE and upright T waves in V1-V4, with appropriate T wave inversion and STD in V6, I, and aVL. Many would call this "LVH with strain pattern." If the QRS were normal, this pattern of STE and large T waves in V1, with STD and T wave inversion in V6, could have been indicative of LAD occlusion.
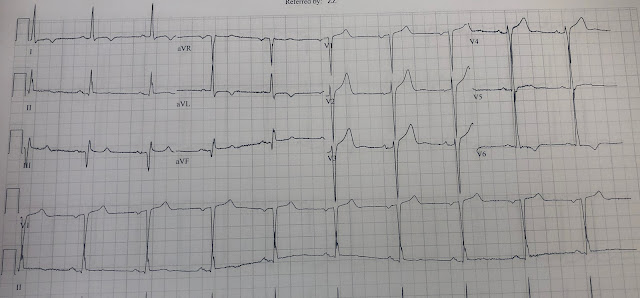
There was a baseline ECG available on file from many years ago:
 |
| I understand that there are differences between the baseline and the current ECG. The T waves are slightly taller in proportion to their QRS complexes. The T waves in V1 and V6 are flipped compared to prior (there is not much LVH "strain" on this older ECG). But my opinion is that they are both versions of LVH without clear signs of OMI, and the change between them is also not specific for OMI. Serial ECGs would be able to prove this theory right or wrong. |
The cath lab was not activated.
The clinical impression was acute hypertensive pulmonary edema. (it is somewhat unusual in my experience that such a patient would not be tachycardic on arrival, but who knows, maybe they were on a beta blocker).
He was treated for this and dramatically improved within the hour.
His initial troponin T was less than 0.01 ng/mL (undetectable, normal less than 0.01 ng/mL), and his serial troponins over the next 12 hours peaked at 0.03 ng/mL, then fell. This would be an extremely low peak level of troponin even with a brief LAD OMI.
Angiogram was not performed during this visit.
Serial ECGs were reportedly performed, but not available. The progress notes described the ECGs as remaining unchanged. (this is important, because if the patient had suffered transient subtle anterior OMI, then we would likely have seen anterior reperfusion changes including deepening terminal T wave inversions).
He improved and was discharged home.
It is extremely unlikely in my opinion that his presentation represented OMI (but theoretically still possible and not ruled out by the information above).
Learning Points:
ST segments and T waves can ONLY, EVER be properly interpreted in the context of the QRS that made them. Everything on the ECG is always proportional. Evaluation of raw ST or T wave voltage without consideration of the QRS is useless.
EMS 12-lead ECGs often have a voltage cutoff that may affect visualization of the QRS. This becomes especially important and tricky for patients with LVH, LBBB, etc., who may suffer a false positive cath lab activation due to this effect.
Expert electrocardiographers understand that there can be some differences from a baseline ECG that do not have acutely important meaning. The idea that "baseline ECGs" should remain perfectly static over time is a beginner's concept that the intermediate learner quickly understands to be an oversimplification. In actuality, patients have some fluctuation in their ECG even under normal conditions, change with time, and exaggeration by many clinical features such as tachycardia, hypertension, etc.
Retrospective adjudication of the presence or absence of OMI can be tricky and requires understanding many aspects of the clinical presentation, serial ECGs, troponins, cath findings, etc. This is especially true when no cath was done, however even a "negative" cath doesn't rule out OMI. The case above is one in which many ancillary data points make me quite sure there was not OMI. Most importantly, OMI is NOT defined or adjudicated solely based on an ECG finding - that would be a ridiculous way to classify MIs - and that's why the name OMI doesn't say anything about the ECG! Its about the patient's actual pathophysiology that we are trying to identify and treat!!!


No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.