A 60-something woman with h/o bioprosthetic MV replacement and COPD, who is not on anticoagulants (bioprosthetic valves generally do not require anticoagulation), presented after 14 hours of left sided chest pain with radiation down left arm. It woke her up at 0200. She states that now it is worse with deep inspiration and associated with SOB.
Here is her triage ECG:
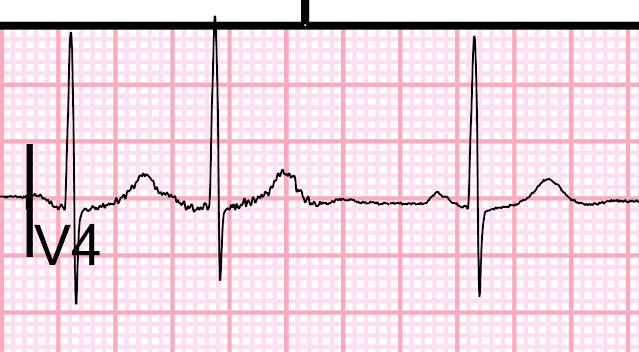
Here I magnify leads V2-V4:
Most individuals, at baseline, have ST Elevation in V2 and V3. It is rare to have ANY baseline ST depression.
This 2001 paper by Peter MacFarlane proves the point:
Macfarlane PW. Age, sex, and the ST amplitude in health and disease. J Electrocardiol [Internet] 2001;34 Suppl:235–41. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11781962
In this paper, Dr. MacFarlane establishes that 97.5% of apparently healthy females over age 50 (or any age, really) have ST amplitude in lead V2 of greater than -0.2 mm (0.2 mm STD), and in V3 and V4 of greater than -0.5 mm (0.5 mm STD), as measured at the J-point, relative to the QRS onset. See table pasted below.
In other words, ANY ST depression greater than 0.2 mm in V2, or greater than 0.5 mm in V3/V4, is abnormal and is suspicious for ischemia, whether posterior MI or subendocardial.
For men of ANY age, almost 100% of apparently healthy individuals have no ST depression in V2-V3 on baseline ECG.
We (Pendell Meyers and Alex Bracey and others) have a paper in consideration at JAHA that shows that, for patients who present with symptoms of ACS, ANY ST depression in V1-V4 is highly specific for OMI. When it is published, we will share it.
Clinical Course
The ED was extremely busy, and the patient was placed in triage and a troponin was ordered:
The first troponin returned at > 50,000 ng/L.
Patient was taken to cath lab:
Acute MI, NSTEMI.
Culprit is 99% Thrombotic occlusion of the first Obtuse Marginal. The rest of the coronaries were normal, and the morphology of the thrombotic occlusion was highly suspicious for an extra-coronary source of embolization. The lesion was reduced to 0% with thrombectomy only, there was no need for PTCA or stenting as I think the culprit is not a ruptured plaque that needed scaffolding.
In other words, it was an OMI NSTEMI [STEMI (-) OMI] due to embolism from mechanical valve since patient was not taking her anticoagulants.
Echo showed:
Regional wall motion abnormality-anterolateral. Regional wall motion abnormality-inferolateral (this is what is reported for posterior wall motion abnormality)
Trans-esophageal echo (TEE) showed a mobile mass on the annulus of the bioprosthetic mitral valve, probable source of the embolus. There was also a high gradient (11 mmHg), pulm hypertension, and no evidence of vegetation (no endocarditis). The patient will likely need MV replacement again, and was started on anticoagulation.
Comment:
I think few providers would notice this very subtle ST depression.
Fortunately, this delay had no serious consequences because the damage was already done. However, this is a large acute MI (a type 2 MI), and she could have arrested in triage.
Learning Point:
When a patient presents with symptoms compatible with ACS, ANY ST depression of any amount, in leads V2 and/or V3, is highly suspicious for ischemia, and if maximal in these leads (as opposed to V5, V6), it is highly suspicious of posterior OMI.
Table from MacFarlane et al (2001)
For each demographic, the top number is mean +/- SD, and the bottom number are 95% confidence intervals. This means that 2.5% of normals have an ST below the level of the first number.



Is there N terminal wave (late depolarisation wave? in inferior leads?
ReplyDeleteIt certainly at least resembles one. good eye!
DeleteQuote " In other words, it was an OMI NSTEMI [STEMI (-) OMI] due to embolism from mechanical valve since patient was not taking her anticoagulants."
ReplyDeleteBut I thought the patient received bioprosthetic valve?
Yes, so this is unusual, but not unheard of.
Deleteincredible Steve.... i an sorry to say that i recently saw a case where there were significant in-your-face ST depressions in V2-3, with chest pain. (sent to me by my brother at another institution). the ED doc just thought it was ischemia , ACS and was admitted to the medical floor. we are just coming out of the Dark Ages, in so many ways.
ReplyDeletethank you for this.
tom
have to confess that I am still not able to confidently see the STD over the precordial leads even after reading your explanation. But what about the inferior leads? I think they also had some STD which looks more obvious to me. Did they affect your interpretation in this case?
ReplyDeletewell, you are right. there is some STD in inferior leads as well.
DeleteDr.Smith
ReplyDeleteReg Dr Smith's ECG BLOG: Tuesday- Aug 3rd 2021.
Congratulations for posting this superb case.
A major infarction lurking behind a totally inconspicuous ( barely 1mm) STD is spotted and patient
is pulled out of the jaws of death by timely intervention - all with evidence based push.
This magical cure is simply phenomenal.
Dr.Smith has been teaching us all along with real world ECGs centering on SUBTLE ECG Manifestations
of ACS through his Book and Blog; but "THIS ONE TAKES THE CAKE". Hats off to you Dr Smith.
With regards,
Dr.R.Balasubramanian
Pondicherry- INDIA