Written by Willy Frick
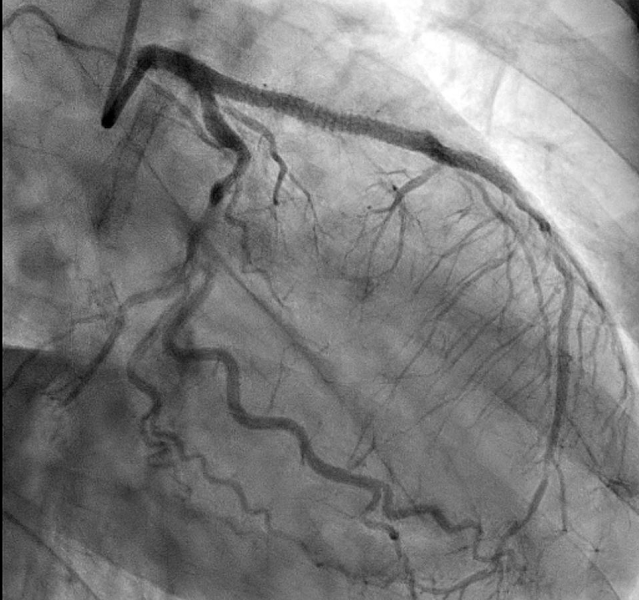
A middle aged man was inspecting the food in his (closed) oven when he felt a few moments of light-headedness. He subsequently woke up on the ground, unsure how long he had been unconscious. He presented for evaluation where inpatient workup including monitoring on telemetry was unremarkable. He was discharged with an event monitor and electrophysiology follow up.
The event monitor lasted for four weeks and showed almost no abnormalities, but the following strip was recorded.
-for%20Willy.png) |
| (From VPS — Connolly et al — JACC, 1999 ) |
-USE.png) |
| (From VPS II — Connolly et al — JAMA, 2003 ) |
- Diagnose phase 4 block, an indication for permanent pacing
- Explain why we do not routinely pace patients with vasovagal syncope
- Review VPS and VPS II, a historical lesson in the importance of sham control
References:
Connolly, S. J., Sheldon, R., Thorpe, K. E., Roberts, R. S., Ellenbogen, K. A., Wilkoff, B. L., Morillo, C., & Gent, M. (2003). Pacemaker therapy for prevention of syncope in patients with recurrent severe vasovagal syncope: Second Vasovagal Pacemaker Study (VPS II): a randomized trial. JAMA, 289(17), 2224. https://doi.org/10.1001/jama.289.17.2224
Connolly, S., Sheldon, R., Roberts, R., & Gent, M. (1999). The North American Vasovagal Pacemaker Study (VPS). Journal of the American College of Cardiology, 33(1), 16–20. https://doi.org/10.1016/s0735-1097(98)00549-x
Lee, S., Wellens, H. J. J., & Josephson, M. E. (2009). Paroxysmal atrioventricular block. Heart Rhythm, 6(8), 1229–1234. https://doi.org/10.1016/j.hrthm.2009.04.001
Pillai, A., Ellenbogen, K. A., & Padala, S. K. (2021). A tale of 2 blocks. Circulation, 143(10), 1062–1065. https://doi.org/10.1161/circulationaha.120.052981
MY Comment, by KEN GRAUER, MD (2/4/2025):
- As per Dr. Frick — the primary cause of one or more abrupt pauses with PAVB is a result of a diseased His-Purkinje system. That today's patient may be predisposed to this disorder is suggested in Figure-1 by: i) Obvious QRS widening on this single-lead ECG monitoring strip (suggesting some form of bundle branch block); — and, ii) 1st-Degree AV Block of conducted beats (PR interval ~0.26 second).
- Although the continuous rhythm strip in Figure-1 does not manifest slowing of the atrial rate prior to onset of the ventricular pause (ie, the atrial rate is fairly constant at ~66/minute in the first 2 lines of the rhythm strip) — there is a change in the atrial rate after the return of 1:1 AV conduction (in the form of slight acceleration of the atrial rate to ~81/minute for 6 beats — until resumption of the slower atrial rate at the end of the 3rd line). So, perhaps a component of vagal influence may be operative after all? (ie, 1st-degree AV block — and some rate variability).
- "Devil's Advocate" — Beat "Y" actually looks like a fusion beat (intermediate in morphology between sinus-conducted beats and early ventricular beat "X" ) — which if true, would make for an immediate "reset" of His-Purkinje conduction.
- PAVB is characterized by the sudden, unexpected onset of complete AV block with delayed ventricular escape — therefore resulting in a potentially prolonged period without any QRS on ECG. Prior to the prolonged pause — the patient manifests 1:1 AV conduction without other evidence of AV block (which is why onset of PAVB is typically so unsuspected! ).
- Because of its totally unexpected onset and propensity to result in sudden death — PAVB is difficult to document and significantly underdiagnosed.
- Three mechanisms for producing PAVB have been described: i) Vagally mediated (ie, Vagotonic Block — as described in the January 31, 2019 post, — and in more detail HERE — with the references listed at the end this Blog post citing instances of transient asystole from excessive vagal tone!); ii) Intrinsic (Phase 4 = pause- or bradycardic-dependent) PAVB; — and, iii) Idiopathic.
- The problem with vagotonic PAVB is localized to within the AV Node.
- There will often be a "prodome" of diaphoresis, nausea, dizziness — with the patient aware of imminent fainting.
- Characteristic ECG findings of vagotonic PAVB include progressive sinus rate slowing — often associated with an increasing PR interval and a narrow-QRS escape focus — followed by recovery with progressive return to a normal sinus rate and normal PR interval.
- PD-PAVB appears to be the primary mechanism for the cardiac rhythm in today's case (albeit potential for some vagal contribution given variability in the atrial rate in Figure-1). As per Dr. Frick — the underlying pathology of PD-PAVB is severe His-Purkinje System disease (supported by the finding of QRS widening with conducted beats in today's rhythm strip). This form of PD-PAVB is likely to be fatal unless the patient receives a permanent pacemaker.
- As is superbly shown by Dr. Frick's case — the interesting pathophysiology of PD-PAVB results from chance occurrence of an "appropriately-timed" PAC or PVC that partially depolarizes the diseased HPS (His-Purkinje System) at a specific point in the cycle that renders the poorly-functioning HPS unable to complete depolarization. The resultant prolonged pause in ventricular depolarization may only resolve if another "appropriately-timed" PAC or PVC occurs at the precise point needed to "reset" the HPS depolarization cycle (which presumably explains why the patient in today's case spontaneously recovered).
- Of note — although QRS widening and 1st-degree AV block is seen for conducted beats in today's case — up to 1/3 of patients with PD-PAVB do not show evidence of conduction defects on ECG. This complicates documentation and explains why it is so easy to miss the diagnosis.
- The baseline ECG before idiopathic PAVB tends to be normal.
- No "trigger" for PAVB is evident (ie, no source of excessive vagal tone — and no precipitating PACs/PVCs are seen).
- It is fortunate that this patient was monitored over an extended period of time ( = 4 weeks). It is humbling for me to see how easily the diagnosis could have been missed in today's patient.



-USE.png)








-USE.png)
-USE.png)