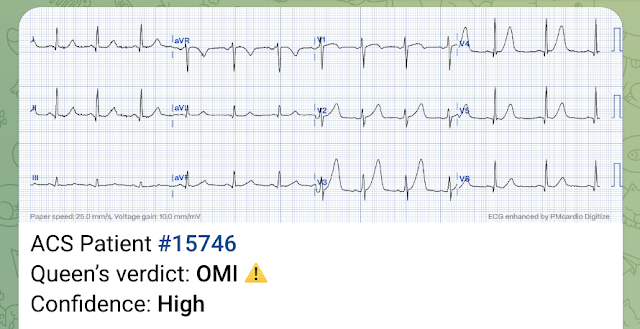
I have collected 51 OMI cases that were diagnosed as completely normal by the conventional automated computer algorithm.
Shifa Karim and Gabe Keller helped with a project to assess all these ECGs with the Queen of Hearts.
Part of the result is back:
Of those 51 cases of OMI with a "completely normal" ECG (not even "nonspecific ST-T abnormalities, but completely normal!), 35 were diagnosed by the Queen of Hearts as OMI.
I wanted to show some of the cases here.
You can read all the details in the links if you want.
The Queen of Hearts PM Cardio App is now available in the European Union (CE approved) the App Store and on Google Play. For Americans, you need to wait for the FDA. But in the meantime:
Or use the QR code:
10 Cases:
Case 1
Do you want to be interrupted to view what the computer calls normal or nonspecific ECGs? 2 cases at once!
Case 2
A middle-aged woman with chest pain and a "normal" ECG in triage. The OMI was not seen and she arrested in triage.
Case 3
Should Emergency Physicians be interrupted by ECGs that are read as "Normal" by the computer?
Case 4
How unreliable are computer algorithms in the Diagnosis of STEMI?
Case 5
Subtle Dynamic T-waves, Followed by LAD Occlusion and Arrest
Case 6
An Elderly Male with "Indigestion"
Algorithm is either Glasgow or Marquette 12 SL |
Case 7
Chest pain relieved by Maalox and viscous lidocaine. Diagnosed as Normal by the computer. Troponin negative. Patient was being discharged with a diagnosis of GERD when he arrested.
Unknown algorithm
Case 8
Another Inadequate Paper Published on Triage ECGs, whose Conclusions Need Scrutiny.
Case 9 (prehospital and ED ECGs).
Echocardiography, even (or especially) with Speckle Tracking, can get you in trouble. The ECG told the story. 30 yo woman with trapezius pain. HEART Pathway = 0. Computer "Normal" ECG. Reality: ECG is Diagnostic of LAD Occlusion.
- As we have so frequently documented on Dr. Smith's Blog for well over a decade now — all-too-many clinicians (including all-too-many cardiologists) — remain "stuck" in the STEMI Paradigm, as well as ignoring increasing data in support of cardiac cath-validated studies showing at least 30% of acute OMIs (Occlusion Myocardial Infarctions) are missed if one depends solely on millimeter-based criteria from the outdated STEMI Paradigm.
- The above said — the fault is not in the computer — since computer programs merely do what they are programmed to do.
- Conventional ECG interpretation programs (ie, virtually all computer interpretation programs prior to the QOH AI Bot app) — have been programmed according to STEMI criteria — without consideration of clinical context (ie, correlation of the presence and relative severity of symptoms with each of the serial ECGs that are done) — and without consideration of the additional ECG findings that we routinely emphasize on this ECG Blog that correlate with OMI (See Figure-1).
- As a result — We should not expect conventional ECG interpretation programs to manifest even a reasonable degree of accuracy for recognizing acute OMI. And, as a result — We should not be using conventional ECG interpretation programs for this purpose.
- Finally — Clinicians (including cardiologists) who in 2024 remain "stuck" in the STEMI Paradigm (and who continue to ignore other ECG findings shown to more reliably identify acute OMI, as noted in Figure-1) — such clinicians will continue to delay (if not completely overlook) the need for prompt cardiac catheterization of acute OMIs that could (and should) benefit from prompt revascularization.
- Optimal clinical ECG interpretation for identification of acute OMI can be attained by attention to the principles reviewed in the 90-minute Webinar by Drs. Smith, Meyers and Herman (in the December 5, 2023 post of Dr. Smith's ECG Blog) — many of which are summarized in Figure-1 — and, all of which are routinely discussed in cases presented on this ECG Blog.
- The QOH (Queen Of Hearts) PMcardio OMI AI model offers proof that the fault of conventional ECG interpretation programs is not the fault of the computer. On the contrary — because QOH has been programmed through guidance by Drs. Smith and Meyers (with an ever expanding data base of more than 18,000 tracings with cath-finding validation) — QOH already manifests superior accuracy for identifying acute OMI compared to the use of standard STEMI critieria (Herman, Meyers, Smith et al — Eur Heart J Digital Health — November, 2023).
- MY Thought: Optimal clinical ECG interpretation will probably be BEST attained by a combination of expertise from experienced clinicians with the already impressive, but continually improving accuracy of QOH. Some degree of clinician oversight will probably always be needed to ensure optimal performance of QOH — but the additional opinion QOH provides can clearly be of great assistance to clinicians as a teaching tool, and for increasing clinician confidence and accuracy for rapid identification of which patients need prompt cath.
.png) |
| Figure-1: ECG findings to look for when your patient with new-onset cardiac symptoms does not manifest STEMI-criteria ST elevation on ECG. For my clarifying Figure illustrating T-QRS-D (2nd bullet) — See My Comment at the bottom of the page in Dr. Smith’s November 14, 2019 post. |
- The March 31, 2023 post —
- The February 4, 2022 post —
- The May 23, 2023 post —
- Never look at what the computer says until after you have forced yourself to interpret the patient's ECG in conjunction with available clinical information.
- Only THEN — Look at what the computer said. Do you agree?
- Realize that IF the program available to you is based on a conventional ECG algorithm — that these are not reliable programs for identification of acute OMI (ie, Far too many false positives and false negatives!).
- IF you do have availability of QOH — You can feel reassured IF your clinical impression matches that of QOH.
- IF on the other hand, your interpretation differs from that rendered by QOH — GO BACK to the drawing board, realizing that unless you can come up with a valid reason for why QOH may be mistaken (ie, artifact, your availability of serial or prior tracings) — that the QOH AI app is usually accurate.
- Keep in mind that the QOH PMcardio OMI AI model will continue to get better as it gets programmed with thousands of additional ECGs (all with cath-validated data) — and as QOH becomes capable, as it will with time — of integrating prior and serial tracings, as well as historical information into its interpretations.
























No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.