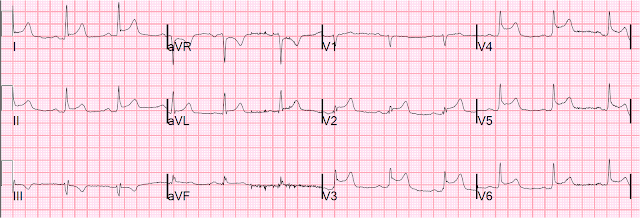
An over 90 yo patient complained of 1 hour of chest pain. There was a h/o CAD with CABG. The prehospital BP was 200 systolic. The paramedics recorded an ECG which could not be obtained but which was identical to the ED ECG recorded here:
The paramedics activated the cath lab. The CP resolved with NTG and ASA, and the ED BP was 170/90. She was given heparin and abciximab and taken to the cath lab. There were several severe chronic calcified lesions, no culprit, and no PCI was performed.
However, there were severe bleeding complications and she died of a retroperitoneal hemorrhage.
There are several lessons one can be reminded of by this case:
1. Not all ST elevation is acute STEMI
2. Acute STEMI usually has large T-waves and, unless anterior, does not develop Q-waves rapidly. When you see inferior or lateral QR-waves, think of old MI with persistent ST elevation.
3. Hypertension can cause ischemia with chest pain
4. If the pain goes away and the ECG is equivocal, then slow down
5. PCI has risks, mostly bleeding risks, and these are much higher in the elderly, especially women
Summary of this case:
ECG differentiation of old vs. new MI is frequently difficult, so assess risks and uncertainties:
Bleeding Risk Factors in PCI
GRACE registry 24000 patients; Eur Ht J 24:1815; 2003
Major bleeding definition: life threatening:
Assess risk benefit
Be more certain of diagnosis
High risk vs. lower risk STEMI
However, there were severe bleeding complications and she died of a retroperitoneal hemorrhage.
There are several lessons one can be reminded of by this case:
1. Not all ST elevation is acute STEMI
2. Acute STEMI usually has large T-waves and, unless anterior, does not develop Q-waves rapidly. When you see inferior or lateral QR-waves, think of old MI with persistent ST elevation.
3. Hypertension can cause ischemia with chest pain
4. If the pain goes away and the ECG is equivocal, then slow down
5. PCI has risks, mostly bleeding risks, and these are much higher in the elderly, especially women
Summary of this case:
ECG differentiation of old vs. new MI is frequently difficult, so assess risks and uncertainties:
Risks:
Age
Uncertainty:
Q-waves
Known previous MI with CABG
Chest pain resolved.
BP 200 systolic
Bleeding Risk Factors in PCI
GRACE registry 24000 patients; Eur Ht J 24:1815; 2003
Major bleeding definition: life threatening:
- Transfusion of ≥2 units PRBC or
- Decrease in hematocrit of ≥10% or
- Intracranial hemorrhage or
- Death
- 4.8% in patients with STEMI
- 4.7% in patients with Non-STEMI
- Advanced age
- Female sex
- History of bleeding
- Renal insufficiency
- (Diabetes and stroke in other studies)
- After adjustment, major bleeding is:
- Significantly associated with increased risk of hospital death (OR 1.64, 95% CI: 1.18, 2.28).
- Also: Transfusion is associated with worse ischemic outcomes!
Assess risk benefit
Be more certain of diagnosis
High risk vs. lower risk STEMI
- Anterior vs. other locations
- Poor LV function on echo
- Hemodynamics (shock, blood pressure, pulse)
- Pulmonary edema
- ST score (how many leads involved? How widespread?)
- Ongoing symptoms (vs. resolved)
- Resolution of ECG findings associated with much lower risk
Appropriate dosing of Heparin
60 U/kg Loading dose: IBW + 0.4(TBW-IBW), maintenance 12 U/kg/hr: IBW + 0.4(TBW-IBW)
Use of bivalirudin
60 U/kg Loading dose: IBW + 0.4(TBW-IBW), maintenance 12 U/kg/hr: IBW + 0.4(TBW-IBW)
Use of bivalirudin
- (always with clopidogrel) vs. heparin + abciximab
- HORIZONS-AMI, 3 yr outcome, 2011
- Lower mortality (5.9 % vs. 7.7%)
- Lower cardiac mortality (2.9% vs. 5.1%
- Lower major bleeding (6.9% vs. 10.5 %)
- ISAR-REACT 2011
- No difference in ischemic outcomes or death
- Major Bleeding 4.6 % vs. 2.6%
Radial artery access
Clopidogrel 300 mg, vs. 600 mg, vs. Prasugrel, vs. Ticagrelor (the latter have less ischemia, more bleeding)