I was called to the resuscitation room to manage a STEMI patient.
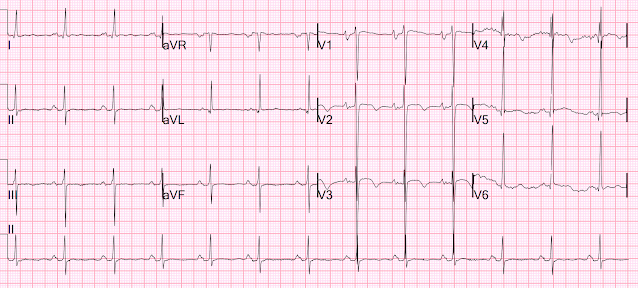
I walked into the resuscitation area and was handed this ECG:
Within 3 seconds, I said: "That is a Fakeout". (i.e., a STEMI mimic)
Everyone was perplexed. This patient had presented with chest pain and had ST Elevation and they were certain this was a STEMI and they were going to activate the cath lab.
Interestingly, my very smart partner Richard Gray who also reads all my blog posts, was working in triage and had already seen this ECG just as it was recorded, and immediately recognized this as a STEMI mimic. He went to the chart and found old similar ones:
6 months prior
Dr. Gray recognized the triage ECG as a STEMI mimic, and had triaged the patient to the Non Resuscitation area, knowing that this was not STEMI or OMI.
History
I talked to the patient and he stated that he had some mild chest pain now. Dr. Gray related that that the patient's most significant chief complaint was dyspnea, not chest pain. I went into the chart and saw that the patient had a previous diagnosis of heart failure. Given that the vast majority of patients with heart failure have had an angiogram, I looked for it and 9 months earlier he had had a negative angiogram ("no angiographically obstructive coronary disease"). He had a non-ischemic cardiomyopathy, suspected to be due to hypertension. The BP on this day was not very elevated even though he was off of his medications.
We recorded another ECG at 90 minutes:
Chart review:
H/o CM probably due to hypertension
Angiogram negative 9 months prior -- negative
Echo 9 months prior:
Mild left ventricular enlargement.
Normal left ventricular wall thickness.
Severely decreased left ventricular systolic function with an estimated EF of 13%.
No regional wall motion abnormality.
Restrictive left ventricular filling pattern consistent with elevated left-sided pressures.
Right ventricular prominence and severely decreased right ventricular systolic function.
The first high sensitivity troponin I was 30 ng/L (Abbott Architect, URL = 34 ng/L for men, 16 for women), then at 2 hours 31 ng/L, then 26 ng/L at 4 hours. MI ruled out.
Even if the troponin had been above the URL (in the range of 35-100 ng/L, I would have suspected that it is due to chronic myocardial injury, or acute myocardial injury due to acute exacerbation of heart failure.
Next AM while still in the ED having his mild heart failure exacerbation treated in the overcrowded ED:
He was discharged.
Learning Points: How did I know that this was a STEMI mimic?
--Because I recognized ECGs like I recognized faces. I have seen this often and know what it is. One must look at a lot of ECGs, look at many known OMIs and known mimics, in order to recognized what is, and what is not, OMI.
Understanding this pathognomonic ECG would have greatly benefitted the patient.
See these cases of the combination of ST Elevation from LVH and Benign T-wave inversion, most of which were false positive cath lab activations. (The 4 ECGs below were all non-ischemic!)
===================================
MY Comment, by KEN GRAUER, MD (10/4/2022):
===================================
- In the hope of enhancing our rapid recognition abilities — Dr. Smith has added to his discussion above, a number of cases illustrating some variations of combined ST elevation + LVH + benign T wave inversion. There are many "flavors" of this type of benign tracing — so the more examples we see — the easier it becomes to recognize that the ECG in front of you showing ST elevation with T wave inversion in a number of leads is not a tracing that merits cath lab activation!
- For readers in search of more practice tracings — the March 22, 2022 post by Dr. Meyers presents a rapid succession of 18 additional "flavors" of BTWI (Benign T Wave Inversion). To this — My Comment at the bottom of the page in this March 22 post adds a "deep dive" on why the initial ECG in that case is benign.
- NOTE: I've added an ADDENDUM below on this page (with illustration in Figures-2 and -3) — in which I consolidate KEY points from a review by Dr. Smith regarding those ECG features that suggest a certain pattern of ST elevation with T wave inversion is likely to be benign.
- To do this — I've reproduced and labeled the 1st and 3rd ECGs shown above in Dr. Smith's discussion (Figure-1).
- Why is ECG #1 not suggestive of an acute OMI?
- Why is the amount of ST elevation less in ECG #3 — that was obtained just 90 minutes later?
- Although we never learn the age of this patient — the increase in QRS amplitude in the chest leads is extreme. Regardless of age — voltage criteria for LVH are easily exceeded.
- Q waves — Small and narrow Q waves are seen in 4 of the lateral leads (ie, in leads I,aVL; V5,V6). Given the size of R waves in these leads — the depth of these Q waves is not excessive (ie, they are normal “septal” q waves).
- R Wave Progression — There is delayed Transition in the chest leads — since the R wave does not become taller than the S wave is deep until between leads V4-to-V5 (Transition usually occurs between V2-to-V4). That said — each of the anterior chest leads ( = V1-V4) manifest a definite r wave, so slightly delayed Transition is not of concern.
- ST-T Wave Appearance in the Chest Leads — There is 2-2.5 mm of ST elevation in leads V1-V3. ST segments remain coved, with a lesser amount of ST elevation in leads V4,V5 (and perhaps trace ST elevation in V6). There is a hint of beginning T wave inversion in leads V1-3 — and definite terminal T wave inversion in leads V4,V5.
- In the Limb Leads — The ST segment in lateral leads I,aVL resembles the appearance in lead V6. The ST segment in the inferior leads is coved (albeit not elevated) — with several millimeters of symmetric T wave inversion.
- As noted above — QRS amplitude in the chest leads is huge! (ie, S waves >25 mm are seen in 4 successive anterior leads — and the R wave in lead V6 is ~25 mm). As a result — the relative amount of anterior ST elevation seen in leads V1-V3 is clearly not disproportionate considering this dramatic increase in QRS amplitude. If anything, the amount of anterior ST elevation is less than I would expect in a patient with this much LVH.
- NOTE: For more on the concept of proportionality and LV "strain" appearing as anterior ST elevation — See My Comment at the bottom of the page in the June 20, 2020 post in Dr. Smith's ECG Blog.
- The T wave inversion in ECG #1 is most prominent in the mid-chest leads (as well as being seen in the inferior leads). This distribution is perfectly consistent with Dr. Smith’s synthesis of those ECG characteristics typical for STTNV ( = the Normal Variant pattern of ST Elevation with T wave inversion) — as I summarize below in Figure-2.
- The QTc is relatively short (ie, ~0.40 msec.).
- Distinct J-point notching is seen in lead V5 (with terminal R wave “slurring” in lead V6).
- Those chest leads with T wave inversion manifest some ST elevation.
- T wave inversion is most prominent in leads V4,V5 (which is more lateral than is usually seen with Wellens' Syndrome).
- T wave inversion is seen in the inferior leads.
- R wave amplitude is significantly increased in lateral leads (and the S wave is minimal in lateral lead V5 that shows ST elevation and T wave inversion).
- To The Above — I'd add: i) There is no loss of anterior lead R wave size (as is often seen in patients with evolving LAD occlusion); ii) The tremendous increase in QRS amplitude in so many leads is all but 'screaming' — "I have LVH!" — and, iii) As per Dr. Smith — with experience, this ECG has a "face" that I have seen often and recognize as LVH with ST elevation and T wave inversion that is not due to acute coronary occlusion.
- There are several reasons why this general truism does not hold in today's case!
- QRS morphology in the chest leads has significantly changed in the 90 minutes since ECG #1 was recorded. Specifically — i) S wave depth in leads V1,V2 of ECG #3 is now much less (ie, 16 and 13 mm — compared to 27 and 38 mm in ECG #1); ii) QRS amplitude in lead V4 has been reduced to a small, isoelectric complex in ECG #3 (within the dotted BLUE rectangle). In contrast — the S wave was still huge in lead V4 of ECG #1; and, iii) R wave amplitude has become much larger in lead V5 of ECG #3.
- The P waves in leads V1,V2 of ECG #1 were biphasic — with a definite initial positive deflection (ie, within the BLUE circles in ECG #1).
- In contrast — the P waves in leads V1,V2 of ECG #3 are all negative! (ie, within the RED circles in ECG #3). In addition to reduced S wave size — the shape of the QRS complex in leads V1,V2 of ECG #3 now closely resembles the shape of the QRS complex in lead aVR (whereas the shape of the QRS complexes in leads V1,V2 of ECG #1 looked nothing like the shape of the QRS in lead aVR of that tracing!).
- PEARL — As I emphasize in My Comment at the bottom of the page in the April 17, 2022 post in Dr. Smith's ECG Blog — the above features strongly suggest that leads V1,V2 in ECG #3 were malpositioned (probably 1-2 interspaces too high). I strongly suspect that the reason for change in the amount of ST elevation between the 2 ECGs in Figure-1 — is that precordial lead placement changed!
- The BOTTOM Line in Today's Case: As per Dr. Smith — there is no indication for cardiac cath on the basis of these serial ECGs.
- In Figure-3 — I've adapted 2 illustrative ECGs from the Roukoz & Wang study that compare distinguishing features of ERP and STTNV.
-USE.png) |
| Figure-2: Features of STTNV (Normal Variant of ST Elevation with T Wave Inversion). I've adapted information from the study by Roukoz and Wang (Ann Noninvasive Electrocardiol 16:64-69, 2011) — and from the March 22, 2022 post in Dr. Smith's ECG Blog, which cites KEY ECG findings that Dr. Smith's Review found to be associated with STTNV. |
-USE.png) |
| Figure-3: I've adapted this Figure from the study by Roukoz and Wang (Ann Noninvasive Electrocardiol 16:64-69, 2011) — as it provides superb illustration of ERP (Early Repolarization Pattern) — as compared to STTNV (Normal Variant of ST Elevation with T Wave Inversion). Panel A (TOP tracing) = ERP — in which ST segments are elevated with an upward concavity in leads V3-V6. Note the distinct J-point notching in lead V4 (and very subtly in V5). T waves are upright and tall (especially tall in lead V3). Panel B (BOTTOM tracing) = STTNV — in which ST segments are elevated in all chest leads (but with the distinctive coved shape of STTNV in V2-V6). ST elevation is greatest in V2,V3. There is subtle J-point notching in V2,V3,V4. T wave inversion is seen in 4 of the chest leads that manifest ST elevation (V3-V6). Similar ST coving with subtle T wave inversion is also seen in 4 of the limb leads (including inferior leads II and aVF). |








-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.