Written by Pendell Meyers, additions and edits by Grauer, Smith, McLaren
Below we have 5 cases of adults (ranging from 40-70 years old) who all presented to the ED with acute nontraumatic chest pain that sounded at least somewhat like potential ACS to the provider.
You should look at each ECG and decide if it is OMI, not OMI, or something else.
Our goal in this post is to compare and contrast OMIs with false positives that mimic them. In this post we will examine the anterolateral distribution that has been described as the "South African Flag Sign." (SAFS)
It is very hard to describe why an ECG expert can easily differentiate these 5 cases. Some of these cases will appear to violate some rules of thumb that are commonly given in rudimentary ECG education. In the end, what matters is accuracy - can you tell which are "real" and which are "fake"? For now, the only thing that can tell the difference is expert human interpretation by someone who has spent much time to memorize these ECG patterns and correlate them with patient outcomes.
Think about faces: you can recognize your friend instantly. But can you describe why? Did you measure her nose? The size of her eyes? No. An EKG is like a face and you need to get to know them so you can recognize them. This is what we hope to teach to artificial intelligence.
A short discussion of the SAFS pattern will come at the end for review.
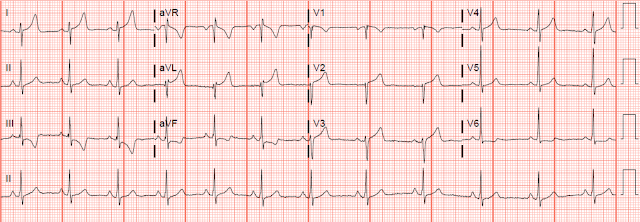
Case 1
Case 2
Case 3
Case 4
 |
Case 5
Scroll down for answer key and discussion.
Case 1 - Normal variant (Not OMI, False Positive STEMI criteria)
With no clinical information at all, I sent this to Dr. Smith who immediately said "Not OMI." I responded: "Correct. But you can see why well meaning learners who are trying to learn to find hyperacute T waves and the south african flag sign are so upset when I told them that!"
ECG: Sinus rhythm. QRS grossly within normal limits. STE in I and aVL and V2, reciprocal STD in III and aVF. The T waves are tall in I and aVL, but not "fat." They are not hyperacute, because they are not "inflated with air" in my opinion. The morphology of the STD and TWI in III is especially specific for NOT OMI, and it has the appearance of LVH with "strain pattern." It is fake, not OMI.
Clinical info: 40s year old woman presented to the ED for off and on chest pain over a week or so, with an episode today that woke her from sleep and wouldn't go away. There was associated cocaine use, but unclear if recently.
Here is an example of a prior ECG on file:
STEMI was activated. Cardiology refused and cancelled the cath lab activation, reportedly stating that they believed that her ECG findings were consistent with prior episodes of cocaine use. I am not quite sure what that means or what exactly their reasoning was, but regardless no angiogram happened.
The patient was admitted to medicine for high risk chest pain.
Three serial troponin I measurements were each 9 ng/L.
Potassium level was 4.1 mEq/L.
She checked out against medical advice before any further workup was done.
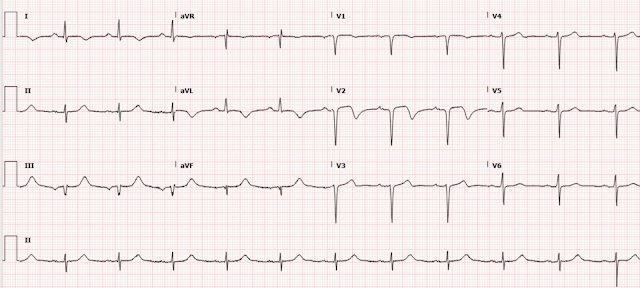
Case 2 - D1 OMI (STEMI[-] OMI)
ECG: Sinus rhythm, QRS grossly normal. Subtle STE in I and aVL, with tiny terminal T wave inversion in aVL. Reciprocal STD in II, III, aVF. V2 has the slightest suggestion of STE with convex ST segment. This one matches many prior cases of true SAFS in my experience, and the morphology looks like acute OMI at least affecting the high lateral leads. The slight terminal TWI in aVL may suggest that it is starting to reperfuse.
Clinical info: 70s year old M with chest pain for 1 hour.
Initial high sensitivity troponin I = 27 ng/L (below the URL; i.e. normal)
Given ASA, morphine, NTG for ongoing pain.
Repeat trop 233, then 14,000, then greater than 25,000 ng/L
As this was not recognized as OMI, cath was done too late and showed 100% thrombotic acute D1 occlusion, stented.
EF 35%, WMA mid-apical anterior, lateral, and apical myocardium.
Post PCI ECG:
Case 3 - D1 OMI (STEMI[-] OMI)
Sent to Dr. Smith with no information at all, who immediately responded with: "This one is OMI."
ECG: Sinus rhythm. QRS grossly within normal limits. Similar to case above with STE in I and aVL with reciprocal STD in III and aVF. Similar V2 as case above. This time the T waves are upright in I and aVL. Leads III and aVF have a very concerning "down-up" morphology that is specific for reciprocal STD from OMI in lead aVL.
Clinical info: 50s year old man with tobacco use presents for acute substernal chest pain just prior to arrival.
Initial troponin less than 6 ng/L (less than limit of detection).
Repeat troponin 17 ng/L.
Echo shows hypokinesis of the anterolateral myocardium.
Repeat trops: 2740, 5835, 7077 ng/L. None further ordered.
Cath shows acute thrombotic occlusion of D1, deemed small and not suitable for PCI.
No further ECGs recorded.
Note: the first 2 troponins were negative; if you rely on troponin to make this difficult diagnosis, you will lose a lot of time and all of the myocardium at risk!
Case 4 - Normal variant (Not OMI, False Positive STEMI criteria)
 |
Sent with no information to Dr. Smith, who said "Not OMI."
ECG: Sinus rhythm. QRS shows relatively high voltage, but maybe not meeting clear LVH criteria. Could also be simply healthy young high voltage. There is STE in I, aVL, and V2, with convex ST segments and reciprocal STD in II, III, aVF with TWI. I strongly suspect these T waves are not hyperacute (unless a baseline ECG later proves me wrong), but instead a confusing baseline variant. There is also terminal T wave inversion in V3-V6, which reminds me somewhat of benign T wave inversion pattern (another normal variant). This ECG simply does not look like OMI in my experience.
See here for many examples of "benign T-wave inversion", just like what you see here in V3-V6
Clinical info: A 50s year old man presented with acute chest pain of several hours duration.
Two ED troponins were less than 6 ng/L.
Many prior ECGs on file over years, including this one:
No other dangerous cause of chest pain was found. He was discharged.
Case 5 - mid LAD OMI (the easiest one of all 5, but still STEMI[-] OMI)
ECG: Sinus rhythm. QRS grossly within normal except poor R wave progression and left axis (possibly could describe as LAFB). Hyperacute T waves in I and aVL and V2, STE in aVL and V2. Reciprocal STD in II, III, aVF (from high lateral OMI) and STD in V3-V6 (appears to become maximal in V6, likely indicative of a component of subendcardial ischemia). Terminal QRS distortion in aVL. This one is OMI.
Clinical info: 50s year old man presents with chest pain waking him from sleep 6 hours ago.
STEMI activated, at cath lab: total mid LAD occlusion, stented.
First trop 12,960 ng/L, none further measured.
Post cath ECGs:
South African Flag Sign:
This is a particular ECG pattern found in OMI cases affecting the anteroseptal / anterior / high lateral walls. It has been described as a territory corresponding often to the first diagonal artery, but of course there is substantial coronary variation and any artery in the anterior and or lateral areas can cause this pattern. See the diagrams above from Littmann et al. (referenced below) for the visual explanation of why the pattern of ECG changes can be remembered using the image of the South African flag.
Here is a diagram by Ken Grauer of the South African Flag sign, from this prior post:
References:
Durant E, Singh A. Acute first diagonal artery occlusion: a characteristic pattern of ST elevation in noncontiguous leads. Am J Emerg Med. 2015; 33:1326.e3-5
Littmann L. South African flag sign: a teaching tool for easier ECG recognition of high lateral infarct. Am J Emerg Med. 2015; 34.
DOI: https://doi.org/10.1016/j.ajem.2015.10.022
 |
| Images from google search. |
Learning Points:
If you use the STEMI criteria to decide which patients need emergent reperfusion, YOU WOULD GET ALL 5 OF THESE CASES WRONG. You would falsely activate the cath lab for 2 patients, and withhold treatment of OMI in the other 3!
It can be difficult to determine OMI from OMI mimics, but this is possible with experience and practice, in which you learn based on memorizing the patterns that correlate with the proven outcomes of OMI.
Expertise can correctly overrule many ECg "rules of thumb." Some of the OMIs above have concave ST segments, and some of the false positive ones have convex ST segments! Many of the false positive cases above indeed have reciprocal findings in inferior leads. Reciprocal findings occur regardless of the reason for focal primary findings. If you learn by seeing many cases and their outcomes, you can see which are true positives and false positives.
The South African Flag sign is a nice teaching tool for the anterolateral OMI distribution.
=======================================
MY Comment by KEN GRAUER, MD (5/11/2022):
===================================
- As per Dr. Meyers — "It is very hard to describe why an ECG expert can differentiate these 5 cases". Words on paper do not suffice — since "the rules" are not always followed.
- Instead — there is an intuitive (unspoken) form of "pattern recognition" that just "happens" — in the same way that an experienced clinician can look at a patient, and in a matter of seconds know the likely diagnosis.
- Clearly — seeing the patient and knowing the history would help in your interpretation of these ECGs. But Drs. Meyers and Smith instantly arrived at the correct interpretation in each case without the benefit of any history.
- As I contemplated each of these 5 cases without the benefit of any history — I found myself looking for 1 or 2 leads that I knew were either not normal — OR — that I really thought looked like a benign repolarization change.
- Then I looked for neighboring (or reciprocal) leads that supported that impression.
- NOTE: The South African Flag Pattern described below by Dr. Meyers adds to the challenge (For more on this pattern — See My Comment at the bottom of the page in the April 8, 2022 post of Dr. Smith's Blog). This is because acute occlusion of the 1st or 2nd Diagonal Branch of the LAD will typically only result in ST elevation in 1 chest lead ( = lead V2) — so you lose the potential benefit of seeing similar abnormal ST elevation in neighboring anterior leads.
-USE.png) |
| Figure-1: I've reproduced Case #2 and Case #3 from today's post. |
- The lead in Case #2 that caught my eye — was lead aVL. The shape of the subtle-but-real ST elevation in this lead is not normal. Adding to my concern is the small q wave, and hint of beginning T wave inversion. This is not the appearance of a repolarization change.
- In view of the abnormal appearance in lead aVL — the subtle ST elevation in lead I (above the dotted RED line in this lead) suggests a similar ongoing process in this other high-lateral lead.
- Confirmation that the lead aVL appearance is likely to be acute — is forthcoming from reciprocal changes in all 3 inferior leads (II,III,aVF). The ST segment straightening that we see in these leads (as per the RED lines) — that then leads up into clearly disproportionately tall T waves (considering the modest R wave amplitude) is not normal.
- Normally — there is slight (1-2 mm) upward concavity ST elevation in leads V2 and V3, that is usually accompanied by an upright T wave. The ST segment coving with slight elevation that we see in lead V2, with hardly any T wave (within the dotted RED rectangle in this lead) — is definitely not a normal appearance for lead V2. Raising suspicion more — is the finding of a QS pattern in both leads V1 and V2.
- T waves in leads V3-thru-V6 all look disproportionately tall and peaked considering the modest R wave amplitude in each of these leads. Support that this finding is abnormal is forthcoming from straightening of the ST segments (RED lines).
- BOTTOM LINE: Awareness that acute occlusion (OMI) of the 1st or 2nd Diagonal may cause ST elevation in lead aVL (sometimes also in lead I) — and only in 1 chest lead ( = lead V2) should prompt this diagnosis for Case #2 until proven otherwise. My suspicion that an acute process was ongoing until proven otherwise in this case — was supported by the finding that ST-T waves in no less than 10/12 leads are clearly abnormal!
- Once again — lead V2 caught my eye, as the shape of the subtle-but-real ST elevation in this lead (within the dotted RED rectangle) — is simply not normal.
- Although a small-but-present initial r wave is seen in leads V1 and V2 of Case #3 — there is no doubt that the ST segment flattening in leads V3-thru-V6 is not normal (especially given the contrast in shape between the subtle ST elevation in lead V2 — and the definite ST straightening in lead V3).
- As opposed to the shape of the elevated ST segment in lead aVL of Case #2 — I was not initially certain in Case #3 from looking at lead aVL alone, that the ST elevation represented OMI.
- That said — the 2 limb leads that caught my eye in Case #3, were leads III and aVF. In both of these leads, in addition to ST depression — was a "down-up" terminal T wave which is distinctly abnormal — and which strongly suggested recent (if not acute) reciprocal change to the ST elevation in lead aVL.
- In view of the definitely abnormal ST-T wave appearance of leads III and aVF in Case #3 — the much more subtle-but-present ST segment straightening that we see in lead II completes the inferior lead pattern of "reciprocal changes".
- Similarly — in view of now knowing that the shape of ST elevation in lead aVL of Case #3 is abnormal — the similar ST-T wave shape in lead I doubtlessly reflects the same ongoing process.
- BOTTOM LINE: Although the "look" of Case #3 is not quite the same as what we saw in Case #2 (Note especially the reduced T wave amplitudes in multiple leads) — the "theme" of Case #3 is similar. That is — Case #3 manifests ST elevation in leads I, aVL and V2 — ST depression in leads III and aVF, with an acute "down-up" T wave pattern — and in total, no less than 10/12 leads with clearly abnormal ST-T waves. Once again — the diagnosis should be acute OMI of the 1st or 2nd Diagonal until proven otherwise.
- Here — the History really helps! Even marked ST elevation is often benign when a young adult is either asymptomatic or presents with atypical symptoms. On the other hand — a worrisome history is clear indication of need for more information plus diagnostic testing (ie, stat Echo during chest pain — troponin — repeat ECGs — search for a prior ECG for comparison). IF in doubt — it is best to be prudent until you can rule out an acute event.
- See the April 8, 2017 post — for a nice review by Drs. Smith and Dunbar of some normal variants with T wave inversion.
- See My Comment at the bottom of the page in the September 11, 2020 post — showing lots of ST elevation in a young adult.
- The August 22, 2020 post — Even repolarization variants may sometimes show "dynamic" ST-T wave changes.
- See My Comment in the November 14, 2019 post — regarding distinction between T-QRS-D (Terminal QRS Distortion) vs repolarization variants.
- There are many others — and we continue to post more!










No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.