The information about the binge drinking made the whole team take a non-urgent approach towards the patient. We took our time to settle the patient into bed, secure IV access and by the time we had a cardiac tracing on the monitor, we had the following vitals: HR - 120 bpm; BP - 100/60 mm Hg; SpO2 - 95% on RA. The patient was given antacids, started on IV fluids including thiamine before getting a 12-lead ECG within 10 minutes of arrival. Our differentials included: ACS, Boerhaave syndrome, Pneumothorax, Pancreatitis & GERD.
The monitor showed upsloping ST segments in II. A 12-lead ECG was immediately obtained:
Interpretation: Sinus tachycardia, with RBBB and LAFB. Concordant STE in V2, V3, I, and aVL. The QRS in V4 is isoelectric, with excessive STE. This pattern in ACS is diagnostic of proximal LAD or even left main occlusion. We have shown perhaps 10-20 cases of this ECG pattern on this blog (see links at bottom)!
ECG POCUS showed anterolateral hypokinesia with an EF of ~40%. It took a while for the team to understand the gravity of this new information and to expedite the further process.
The patient had HTN and DM but was not taking medications; he also smoked cigarettes for many years.
Meanwhile, the patient dropped his saturation and his SBP
tanked to 70. Cardiology was also a bit late as it was a Sunday. The patient was
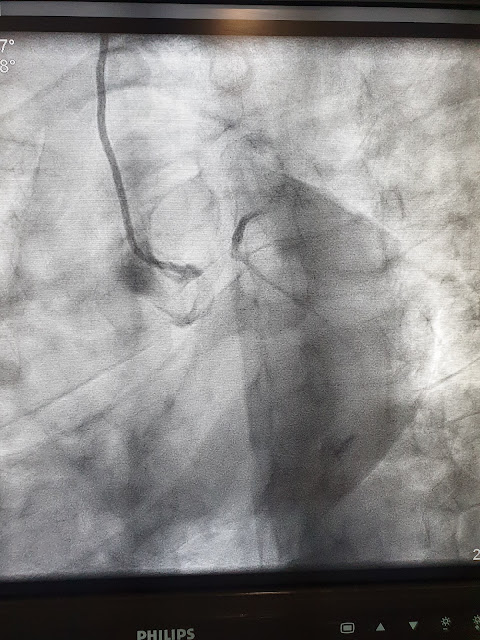
taken to the cath lab approximately 60 minutes after arrival and was found to have a 100% occlusion of LMCA (see image below).
Patient’s initial high sensitivity Troponin-I was found to be "negative": 17 pg/mL = 17 ng/L (the reported reference range for this assay is apparently 0-50 pg/mL or ng/L).
The above angiogram shows a 100% occlusion of the LMCA. There appears to be possible minimal flow or reconstitution of the LAD and LCX.
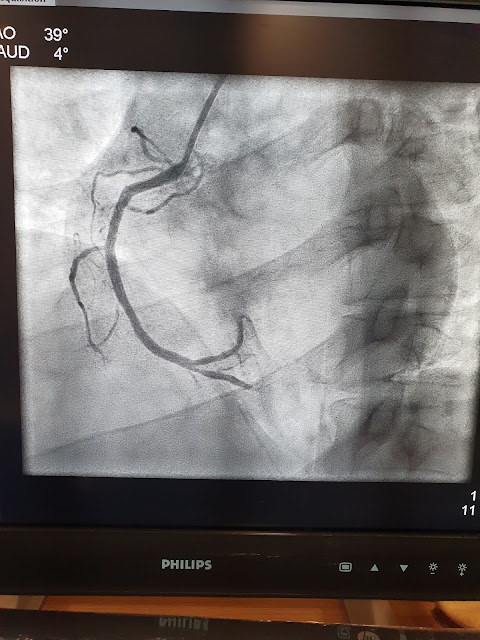
RCA angiogram (above), showing a grossly patent proximal and mid RCA, but which appears to have some distal obstruction.
After PCI of the LM and IABP, the patient coded in the cath lab and was reverted after 2 DC shocks. After another 3 hours in the ICU, the patient had another cardiac arrest and could not be revived. ECMO was not attempted for unclear reasons.
TAKE-HOME POINTS:
Young patients and atypical presentations are important reasons for a delay or missed diagnosis of deadly ACS.
ACS with RBBB and LAFB, usually with some LAD distribution ST Elevation, is diagnostic of proximal LAD or even left main occlusion until proven otherwise. The mortality of such an ECG is very high even before arriving at the cath lab. This is perhaps the highest mortality OMI ECG of all.
You cannot simply hope that an initial high sensitivity troponin will help you realize which patients are high risk ACS and which aren't. A small but important percentage of OMI patients arriving soon after onset of symptoms will have an initial high sensitivity troponin within the normal range. When the troponin is negative or minimal, the benefit of reperfusion is maximal.
Follow up your cases, review their angiograms and clinical outcomes.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.