This is a repost, but it was only posted as a video presentation on hqmeded: https://vimeo.com/18680419
A patient presented with chest pain:
There is an obvious inferior STEMI. The cath lab was activated. I saw the ECG later and called the interventionalist to hear the outcome. He said there was a mid-RCA occlusion. I said, "That is strange, because the ECG has ST elevation in V1 and indicates a right ventricular MI."
He went back to look at the angiogram. He then saw that the culprit was in the proximal RCA, proximal to the RV marginal branch, and that there had, indeed, been an RV MI. The mid-RCA occlusion was an embolus from the proximal RCA. Fortunately, the patient was still on the table and he could go back and place the stent at the correct lesion in the ulcerated plaque in the proximal RCA.
Learning Points:
1. In inferior STEMI, ST elevation in V1 is a very specific finding for right ventricular MI. We have studied this and are near completion of a manuscript on it.
2. In inferior STEMI, it pays to record a right sided ECG.
A patient presented with chest pain:
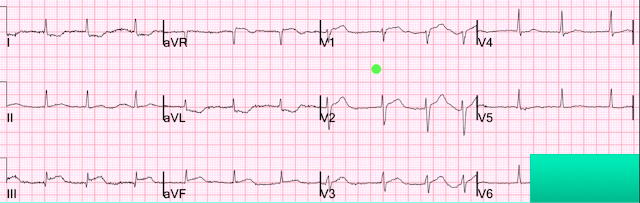 |
| What do you see? (Sorry for the obscured V6. It doesn't show anything) |
There is an obvious inferior STEMI. The cath lab was activated. I saw the ECG later and called the interventionalist to hear the outcome. He said there was a mid-RCA occlusion. I said, "That is strange, because the ECG has ST elevation in V1 and indicates a right ventricular MI."
He went back to look at the angiogram. He then saw that the culprit was in the proximal RCA, proximal to the RV marginal branch, and that there had, indeed, been an RV MI. The mid-RCA occlusion was an embolus from the proximal RCA. Fortunately, the patient was still on the table and he could go back and place the stent at the correct lesion in the ulcerated plaque in the proximal RCA.
Learning Points:
1. In inferior STEMI, ST elevation in V1 is a very specific finding for right ventricular MI. We have studied this and are near completion of a manuscript on it.
2. In inferior STEMI, it pays to record a right sided ECG.

GREAT case! — as it wonderfully illustrates how astute ECG interpretation may tremendously help the angiographer by pointing out WHERE to look for the acute occlusion. Without your astute detection of the likely "culprit artery location" from this ECG, the patient would not have optimally benefited from acute catheterization ...
ReplyDeleteThere are several clues that suggest acute RV infarction (in addition to acute inferior STEMI) on this tracing. Not only is there ST elevation in V1 — but it looks like THE GREATEST AMOUNT of ST elevation takes place in this lead. The ST-T waves in leads V2,V3 are not normal — but they are not as impressive as what I see in lead V1 (whereas with LAD occlusion, we would expect progressively more ST elevation as one moves laterally from V1). In addition — there is relatively more ST depression in lead I than what we normally see at this stage of evolution in acute inferior STEMI — which ALSO suggests some ST depression in lead I in response to acute RV infarction.
THANKS for posting!
a little help:
ReplyDelete- Difference (ECG, RV-extension, Outcome, ...) between RCA-Occlusion prox. to the RV marginal
branch (ramus marginalis dexter, like here) and "more" prox. RCA-Occlusion, for ex. prox. to
the (1.) ventricular branch (ramus ventricularis dexter).
- Is there anyone who studied this difference ? (% of RVMI-extension, free Wall-Septum-ecc.)
toujours merci Dr Smith
Al
Al,
DeleteNot sure what you're asking.
Steve
Great Dr K wang has stressed in his talk- STE in leads II,III, and aVF with STD in leads I and aVL indicate Inferior MI with RV involvement. STD only in lead aVL is Inferior MI with RV involvement. In this ECG there STE in lead V1.
ReplyDeleteGreat case
Jyoti,
DeleteI have studied this and will publish soon: ST depression in lead I does NOT imply RV infarct EXCEPT insofar as it does imply RCA as the infarct artery. But among cases of RCA occlusion, the incidence of ST depression in lead I is the SAME in RV MI vs. No RV MI !!
Steve
I will be very interested to see results of Dr. Smith's study on the subject that Jyoti raises (whenever this study comes out). It was from one of Dr. Wang's talks that my attention was brought to looking closer at lead I. In my anecdotal observations ever since — my thoughts are the following: i) Definitive diagnosis of acute RV infarction depends on right-sided leads ....; ii) Of the standard 12-leads — I may strongly suspect acute RV infarction in certain cases. THIS is one of them for all of the reasons Dr. Smith states above (and the reasons I state in my prior comment); iii) Lead I by itself most definitely cannot and will not reliably predict acute RV infarction; but iv) In certain settings, in which acute RV infarction is suggested by the other 11 leads — the finding of relatively "more" ST depression in lead I than-I-might-otherwise-expect provides a little bit (not a lot) more support that there is likely to be acute RV infarction; and v) The above are fine points with ultimate conclusion only made from an overall Gestalt of complete 12-lead assessment that defies attempts at trying to quantify "criteria for lead I" in words (ie, "a picture is worth 1,000 words"). Anecdotally, the above subtle points have been very helpful to me — but my bet is that there is no hard copy "criterion" for lead I that will reliably indicate acute RV infarction.
DeleteOur data confirms that, on the left-sided ECG, STE in V1 is much more specific to RV infarct than STD in lead I. It is especially specific when there is ST depression in V2 and V3. When there is no ST depression in V2 and V3, it is about 80% sensitive.
DeleteSteve — I could not agree more with your comment!
DeleteI can't see P waves. Is un atrial fibrillation?
DeleteYou are absolutely right! I failed to look at the rhythm!!
Delete