Here is an interesting case just presented in a conference today. Thanks to Dr. Simegn, Asinger, Davies, and Bart for their input.
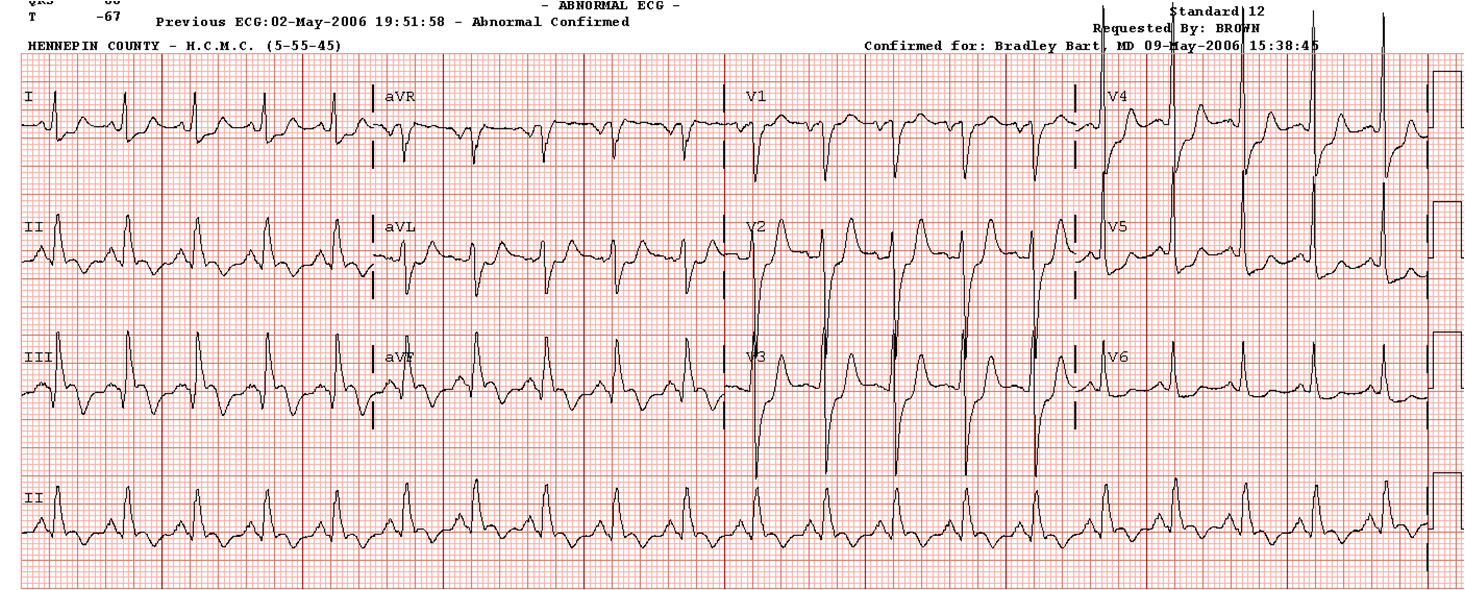
A 69 yo previously healthy woman had very sudden severe dyspnea. The husband at some point reported that they had been physically active that day, and that the patient had complained of some chest pain one week prior for which she did not take his advice to go to the ER. She presented in pulmonary edema, hypoxic on high flow O2, and sats were above 90% on Noninvasive Ventilation. BP was 130/70. Cardiac physical exam was unremarkable except for very coarse breath sounds. ABG was 6.99/44/201/11 on BiPAP. Here is her first ECG:
What else will help you to confirm that this is not atrial flutter, but rather is sinus tachycardia? This is also important because there are notches after the QRS in the limb leads which, if not atrial flutter waves, are ST segment deviation. Is this patient having a STEMI?
The ST segment and QT interval are remarkably short and could easily deceive you into thinking that this is not ST elevation, but rather flutter waves.
Considerations include:
1. Lead V1. In sinus rhythm, the latter part of the p-wave in V1 is always negative, as it represents the depolorization of the left atrium, which is depolarizing away from lead V1. In atrial flutter, the p-wave in V1 is usually upright. Here it looks like a normal p-wave. Furthermore, you don't see an identical wave directly between the p-waves and given that the baseline is pretty steady, it should be there.
2. If flutter, the rate should remain constant in spite of supportive care.
Now that we have established that the rhythm is sinus.
A right sided ECG was recorded 6 minutes later:
A bedside echo showed hyperdynamic function and a large RV. The chest X-ray showed pulmonary edema. The patient's respiratory status deteriorated and she was intubated.
Step back: what caused sudden respiratory failure with pulmonary edema?
--Does acute inferior-posterior STEMI alone do this? Not if the pump function is hyperdynamic.
--Does atrial flutter alone cause severe pulmonary edema in someone who was previously healthy? No. (However, if this is atrial flutter, it is wise to cardiovert and this can only help the situation. This was not done. It appears that the rhythm diagnosis of atrial flutter was not considered. If it is sinus, cardioversion will not hurt.)
--Does massive pulmonary embolism cause pulmonary edema? Rarely, if ever.
A CT pulmonary angiogram was negative.
What test is now indicated? What is the likely diagnosis?
Another ECG was recorded:
It appears that the Q-waves were well formed at the time of presentation.
Posterior STEMI puts patients at risk of papillary muscle infarction and rupture. (The posterior leaflet is supplied by posterior branches off the RCA and is vulnerable, whereas the anterior leaflet has its blood supply from the LAD and circumflex) An infarct in the last several days or one week is consistent with acute papillary muscle rupture. This patient's presentation is classic for acute severe mitral regurgitation.
A 69 yo previously healthy woman had very sudden severe dyspnea. The husband at some point reported that they had been physically active that day, and that the patient had complained of some chest pain one week prior for which she did not take his advice to go to the ER. She presented in pulmonary edema, hypoxic on high flow O2, and sats were above 90% on Noninvasive Ventilation. BP was 130/70. Cardiac physical exam was unremarkable except for very coarse breath sounds. ABG was 6.99/44/201/11 on BiPAP. Here is her first ECG:
 | |
|
What else will help you to confirm that this is not atrial flutter, but rather is sinus tachycardia? This is also important because there are notches after the QRS in the limb leads which, if not atrial flutter waves, are ST segment deviation. Is this patient having a STEMI?
The ST segment and QT interval are remarkably short and could easily deceive you into thinking that this is not ST elevation, but rather flutter waves.
Considerations include:
1. Lead V1. In sinus rhythm, the latter part of the p-wave in V1 is always negative, as it represents the depolorization of the left atrium, which is depolarizing away from lead V1. In atrial flutter, the p-wave in V1 is usually upright. Here it looks like a normal p-wave. Furthermore, you don't see an identical wave directly between the p-waves and given that the baseline is pretty steady, it should be there.
2. If flutter, the rate should remain constant in spite of supportive care.
Now that we have established that the rhythm is sinus.
A right sided ECG was recorded 6 minutes later:
 | |
|
Step back: what caused sudden respiratory failure with pulmonary edema?
--Does acute inferior-posterior STEMI alone do this? Not if the pump function is hyperdynamic.
--Does atrial flutter alone cause severe pulmonary edema in someone who was previously healthy? No. (However, if this is atrial flutter, it is wise to cardiovert and this can only help the situation. This was not done. It appears that the rhythm diagnosis of atrial flutter was not considered. If it is sinus, cardioversion will not hurt.)
--Does massive pulmonary embolism cause pulmonary edema? Rarely, if ever.
A CT pulmonary angiogram was negative.
What test is now indicated? What is the likely diagnosis?
Another ECG was recorded:
It appears that the Q-waves were well formed at the time of presentation.
--Do inferior Q-waves appear immediately after the onset of a STEMI? No. [However, anterior Q-waves (QR-waves) can be present in the first hour after onset of anterior STEMI)].
--The inverted T-waves also argue against an acute and persistently occluded artery.
Therefore, this patient's MI was subacute.
Now, what do you think the diagnosis is?
Posterior STEMI puts patients at risk of papillary muscle infarction and rupture. (The posterior leaflet is supplied by posterior branches off the RCA and is vulnerable, whereas the anterior leaflet has its blood supply from the LAD and circumflex) An infarct in the last several days or one week is consistent with acute papillary muscle rupture. This patient's presentation is classic for acute severe mitral regurgitation.
1. Acute pulmonary edema
2. Hyperdynamic heart (very low afterload out towards the left atrium and pulmonary veins
3. Severe pulmonary edema without hypertension.
4. Evidence of subacute inferoposterior MI (most occur more than 24 hours from onset of MI)
5. Absence of murmur because in acute rupture, the left atrium is small and as the LV contracts, the pressure between the LV and LA rapidly equalize so that there is no lengthy period of turbulence.
An echo with Doppler was the diagnostic study, and confirmed papillary muscle rupture. She was given immediate afterload reduction with nitroprusside, and taken for an angiogram which showed 2-vessel disease and a 90% RCA (the culprit) with flow. Balloon pump was placed and she was taken for immediate valve replacement and CABG and did well.
The initial troponin was 2.4 ng/ml (probably still elevated from the MI one week ago), but did rise to 19 ng/ml by the next morning. After CABG, it rose to 50 ng/ml.

Wow. There is no doubt in my mind that I would've cardioverted this patient.
ReplyDeleteAgree, I thought it was flutter, too. Even if I couldn't find the second p in V1, I thought it was because the waves were smaller than in other leads.
ReplyDeleteAmazing case. I would have liked to see the echo.
But why was the patient so acidotic?
she was in shock from very low cardiac output.
DeleteVery nice case, thank you!:-)
ReplyDeleteI'd have some questions:
1. Why did not the first echo show the mitral regurgitation? (Maybe Doppler is not done routinely during an echo?)
2. I see some ST elevation in V5R and V6R. Not significant, but the QRS amplitude is also small. However, the baseline seems to be wandering.
If it is a true ST elevation, is there RV involvement? Or is it due to acute cor pulmonale?
3. On the first and second tracing there is the questionable deflection after the QRS complex in II, III, aVF. Could it be a blocked atrial premature complex? OK, it is not so likely that it is exactly half way between the sinus P waves, but maybe.
Mitral regurgitation causes left atrial overload, and extrasystoles may arise. Nitroprusside lowered TPR, so the regurgitation fraction and left atrial pressure were also lowered, and so the extrasystoles disappeared (third tracing). Is it correct? What do you think?
Thanks for your answer!
1. It was not a formal echo, they did not look at valves but only at pump function
Delete2. I agree, there is STE in V5R and V6R. I believe it was a proximal RCA occlusion, with RV involvement
3. I don't know, but don't think so. Possible!
Hi Dr Smith,
ReplyDeleteI have problem understanding this particular sentence:
Absence of murmur because in acute rupture, the left atrium is small and as the LV contracts, the pressure between the LV and LA rapidly equalize so that there is no lengthy period of turbulence.
How in acute rupture the left atrium will be small ? How is it different from mitral regurgitation in a patient with dilated cardiomyopathy or a young patient with mitral valve prolapse? I understand the heart sounds but what i would like to know is the physiology in the formation of heart sounds in those three conditions. Thanks
Ryan, If someone has a normal (small) left atrium, then only a small amount of blood need be ejected backwards before the pressure between the LV and LA is equalized. once equalized, there is no more flow and no more murmur, but the pressure is high and it will cause pulmonary edema. Thus, the murmur duration is very short, early systolic.
DeleteIf someone has chronic mitral regurg, likely from chronic slow LV dilatation (cardiomyopathy), then the LA will be large and very distendable, so that more blood needs to be ejected backward in order to completely fill it, equalize the pressure, and stop the flow and thus stop the murmur. So these patients have a long holosystolic murmur.
Steve Smith
What about carotid massage for differential diagnostic of atrial flutter? Thank you for this blog
ReplyDeleteThat might work, though adenosine is more reliable. Thanks!
DeleteSteve Smith
1. This case highlights in the value of bedside echo!
ReplyDelete2. Steve- "posterior" papillary muscle is actually on the "inferior wall", correct? I mean to say: there need not be "posterior" involvement for this muscle to rupture, just inferior. The terminology is quite confusing.
As we discussed, I believe posterior is really posterior.
Delete