Written by Magnus Nossen — with edits by Grauer.
The patient in today’s case is a 30-something female. She has no known previous medical history. Her husband called EMS when the patient experienced new onset seizures accompanied by micturition. The ECG below was recorded by EMS. What is your assessment?
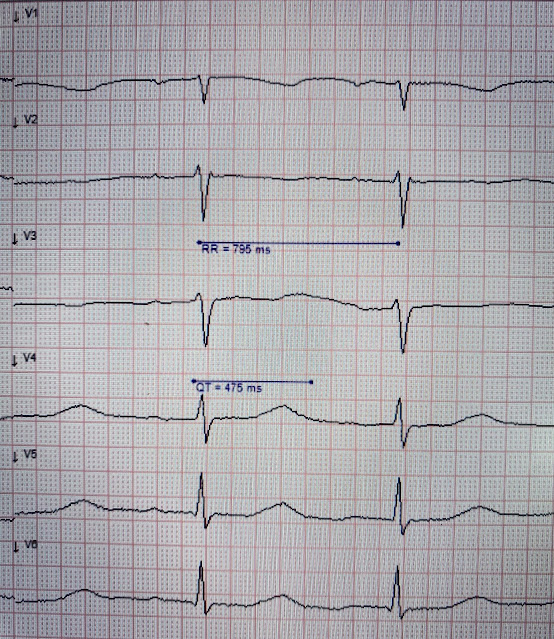
ECG #1
Interpretation: ECG #1 shows sinus rhythm at a heart rate of 77 bpm. The QRS is narrow with a normal PR interval. QRS axis is normal. There is some baseline wander. At first glance, the ECG does not look too abnormal. However, cardiac syncope is always a differential diagnosis when someone presents with first time seizures. In my experience, the pathologic finding in the above ECG is the easiest one to overlook — especially if you are in a rush and do not do a systematic review.
There are a number of things to look for in an ECG that can hint at arrhythmia as the cause of an apparent seizure. Below are some of the conditions to be aware of:
- Preexcitation
- Brugada syndrome.
- Arrhythmogenic cardiomyopathy
- Long QT syndrome
- Hypertrophic cardiomyopathy.
I find it is easier to measure the QTc when the paper speed is 50mm/s, as it is in the image above. I measure the RR interval at 795ms and the QT interval at 475ms. The QTc comes out at 533ms, dangerously prolonged.
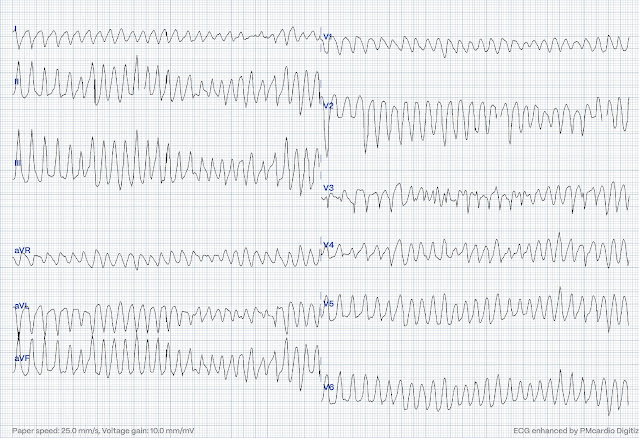
En route to the hospital the patient experienced multiple short-lasting episodes, with cramping and loss of consciousness. She quickly regained consciousness — and was alert in between episodes. One episode was of longer duration. The ECGs below were captured on continuous 12-lead monitoring during transport!
ECG #2
Interpretation of ECG #2:
Underlying sinus rhythm. The sinus beats have a very prolonged QT-interval that seems even longer than in the first ECG. There is a run of polymorphic ventricular tachycardia — which given the QT prolongation, qualifies as Torsades de Pointes (TdP). This run of TdP is initiated by a PVC — but it then self-terminates.
ECG #3
Interpretation of ECG #3:
This rhythm begins as Torsades de Pointes — that then becomes V-Fib. This episode self terminated before defibrillation was possible.
====================================
Discussion: The patient in today’s case presented with "seizures". This case illustrates why all patients with seizures should have an ECG done. This patient was having recurrent episodes of polymorphic ventricular tachycardia with an underlying long QT interval ( = Torsades de Pointes). In the stabilizing area she received 10mmol magnesium sulfate IV, followed by a mantenance drip. Potassium chloride drip was also started. Potassium on admission was 3.5mmol/L (Ref 3.6-4.6) and magnesium 0.88 mmol/L (Ref 0.71-0.94). She stabilized after electrolyte administration with no further episodes of TdP.
- Following more detailed questioning — it turned out the patient had started taking 9 different herbal remedies to ease lethargy and unspecific neurological symptoms. It is unknown exactly what specific herbal medicine and what doses that had been ingested.
Below is a follow up ECG after discontinuation of the herbal remedies. The QTc is significantly shorter. It is very likely that the herbal remedies caused a lengthening of the QT-interval and led to Torsades de Pointes.
In today's case — the QTc shortened after discontinuation of herbal remedies. It is important to be aware that this does not rule out congenital long QT syndrome (LQTS). The QT interval can be normal in patients with LQTS, and sometimes only manifests after a trigger such as hypokalemia or certain drugs.
- The patient did not have a positive family history of epilepsy, sudden cardiac death (SCD) or recurrent syncope.
- Results from genetic testing for LQTS are pending — and the patient has been referred for evaluation of ICD placement.
Learning Points:
- LQTS can have normal QTc.
- All patients with seizures needs an ECG.
- Herbal remedies can potentially be life threatening
See this case for another example of ventricular arrhythmia secondary to herbal medicine.
===================================
MY Comment, by KEN GRAUER, MD (9/2/2024):
===================================
Today's case by Dr. Nossen is fascinating in its complexity — as the patient is a previously healthy young adult woman, whose presentation was with a new-onset Seizure.
- As noted above — the patient had cardiac syncope following a series of episodes of TdP (Torsades de Pointes) — raising the question of whether TdP caused her 1st Seizure — or — if it was the seizure itself that precipitated her malignant arrhythmia? (See Costagliola et al — Ann Clin Transl Neurol 8(7): 1557-1568, 2021 — for more on the complex "Brain-Heart Interaction" in Epilepsy).
- Today's case is further complicated by what I suspect represents body (therefore myocardial) K+ and Mg++ depletion — given the at best "borderline" serum (ECF) levels of these cations reported above in today's case (ie, 3.5 mEq/L for K+ and 1.76 mEq/L for Mg++) — given that ECF levels of these cations comprise only ~1-2% of total body stores (Jahnen-Dechent and Ketteler — Clin Kidney J 5(Suppl 1):i3-i14, 2012 — and — Udensi and Tchounwou — Int J Clin Exp Physiol 4(3): 111-122, 2017).
- Added to this is the fact that today's patient had been taking multiple herbal products for an unknown period of time, with it not known which herbal products were being taken, thereby also being unknown the potential for interactions by possible herbal combinations (See Déléaval et al — HeartRhythm Case Rep 8(5), 2022 — and — Kawatani et al — Oxford Med Case Rep 2023(9), 2023 — for more on potential proarrhythmic effects, including QTc prolongation of herbal products).
For clarity in Figure-1 — I've reproduced the initial ECG in today's case. As per Dr. Nossen — it would be all-too-easy to brush over this ECG as being "unremarkable" — IF one was not routinely systematic in the interpretation of all ECGs they encounter.
- For review of how Systematic 12-Lead ECG Interpretation not only increases accuracy, but also speeds you up — Please check out ECG Podcast #1, with outline and link to my talk on this subject in the July 24, 2024 post in Dr. Smith's ECG Blog.
Regarding my Systematic assessment of ECG #1:
- There is significant baseline artifact, as well as baseline wander. Keep in mind that your interpretation of the ECGs of your patients is part of the medical record. I therefore feel it relevant to document (in your dictation/on the medical chart) when significant artifact potentially impairs the accuracy of your interpretation. Given the importance of accurate measurement of the QT interval in this case — noting there is artifact in ECG #1 is relevant!
- The rhythm in ECG #1 is sinus at ~75/minute.
- Intervals: The PR interval is slightly prolonged (I measure ~0.22 second). The QRS complex is normal (ie, not more than 0.10 second). The QT interval looks to be prolonged (SEE below for details).
- The frontal plane axis is normal (about +70 degrees).
- There is no chamber enlargement.
Regarding Q-R-S-T Changes:
- There appears to be a Q wave in lead aVL (vs an rSr' ) — which as an isolated finding is of uncertain (if any) significance.
- R wave progression is appropriate — with Transition (where the R wave becomes taller than the S wave is deep) occurring normally by lead V4.
- Assessment of ST-T Waves — is challenging, because of the baseline wander and artifact (resulting in changing morphology from 1 beat-to-the-next) — and — because of the nonspecific ST-T wave flattening in multiple leads. However, as shown within the BLUE rectangle in Figure-1 — the end limit of the T wave is clearly seen in leads V4,V5,V6 (the vertical BLUE line in these leads).
KEY Point: The QT interval should be measured in THAT lead in which you most clearly see the end of the QT interval, and, in which lead the QT is longest.
- As shown in Figure-1 — By my calculation, the measured QT = 450 msec. To determine the QTc — We need to correct this 450 msec. value for the patient's heart rate of ~75/minute.
- There are many ways to estimate the QTc (ie, I illustrate a user-friendly method I developed and have used for decades in the October 25, 2023 post).
- PEARL #1: Alternatively — MD CALC is a handy link that provides near instant correction of the measured QT according to heart rate — allowing you to calculate the QTc by any of the 5 most commonly used corrective formulas ( = Bazett — Fridericia — Framingham — Hodges — Rautaharju). Plugging in the above numbers into MD CALC for a heart rate of 75/minute yields results between 476-to-503 msec. for the QTc (depending on which of these 5 formulas you choose). All of these values are clearly over the ~450 msec. that I favor as a "ballpark" upper normal QTc level.
- My Impression of ECG #1: Sinus rhythm at ~75/minute — with nonspecific ST-T wave changes and a prolonged QTc. Because of the baseline artifact and marked variability in ST-T wave morphology from 1 beat-to-the-next — I found it hard to determine if there were (or were not) U waves in ECG #1. That said — in a patient who develops TdP — the overall ECG appearance of this initial ECG is consistent with low K+ and/or low Mg++ (See My Comment in the May 9, 2020 post — for more on the ECG diagnosis of hypokalemia and hypomagnesemia).
- PEARL #2: The principal abnormal finding on this ECG is QT prolongation, here with generalized nonspecific ST-T wave abnormalities. Over the years, I have found recall of a short LIST of Causes of QT Prolongation to be of invaluable assistance. As per My Comment in the March 19, 2019 post of Dr. Smith’s ECG Blog — Assuming there is no bundle branch block, ischemia or infarction (as these entities can prolong the QT) — THINK OF: i) DRUGS (many drugs [including herbal preparations] may prolong the QT interval — and combinations of drugs can result in marked prolongation); ii) LYTES (ie, Think of low K+, low Mg++, low Ca++); and/or, iii) a CNS Catastrophe (ie, stroke, bleed, coma, seizure, trauma, brain tumor).
- Application of the above LIST to Today's Case: All 3 of the categories in the above LIST may be contributing to the QTc prolongation we see in ECG #1: i) Drugs (This patient was taking a number of herbal medications); — ii) Lytes (Probable body depletion of K+ and Mg++ — given low normal serum levels of these cations and generalized nonspecific ST-T wave abnormalities with QTc [or QT-U] prolongation on ECG); — and, iii) CNS (Seizure activity).
- P.S.: For another clinical example of how EASY-it-is to overlook a long QTc if one is not systematic in approach — Please check out the May 3, 2020 post in Dr. Smith's ECG Blog.
-labeled.png) |
| Figure-1: I labeled the initial ECG in today's case. |
The Follow-Up ECG in Figure-2:
The patient in today's case stopped her herbal remedies. Some time after doing so — the ECG shown in Figure-2 was obtained (this being the 4th ECG that was shown above in Dr. Nossen's discussion).
QUESTION:
Dr. Nossen interpreted ECG #4 as showing significant reduction of the QTc after the patient stopped her herbal preparations.
- Instead of a decrease in the QTc — Doesn't return of the T wave to the baseline in lead V3 (at the point just over the RED arrow in this lead) suggest that the QTc is increasing?
-labeled.png) |
| Figure-2: The follow-up 12-lead ECG after the patient discontinued all herbal remedies. Has the QTc decreased? — or is there an increase in the QTc (as suggested by the RED arrow in lead V3)? |
ANSWER:
Rather than highlighting the end of the T wave in lead V3 — I believe the RED arrow in this lead marks the end of a fairly large U wave. Surprisingly — a distinct U wave is not seen in any other lead, which makes it hard to determine what (if any) meaning this single U wave in lead V3 has.
- Determination of the QTc is made by measurement of the longest QT interval that you can clearly see in any of the 12 leads. In Figure-2 — we can clearly delineate the end point of the T wave in most leads. I once again used the last 3 chest leads (within the BLUE rectangle) — with the vertical BLUE line illustrating my measured QT = 370 msec.
- Correcting this measured QT value for a heart rate of ~85/minute — and plugging in these values into MD CALC results between 414-to-440 msec. for the QTc (depending on which of the 5 formulas in MD CALC that you choose).
- CASE Conclusion: The QTc in follow-up ECG #4 shows return of the QTc to normal (as per Dr. Nossen's assessment). Electrolyte replacement — cessation of seizure activity — and stopping herbal preparations all contributed to normalization of this patient's QTc, with improvement of ST-T wave appearance in most leads.
- As per Dr. Nossen — results of genetic testing for LQTS are pending.
- Perhaps this patient may not need ICD placement? — since what appears to be a major causative factor (simultaneous ingestion of 9 herbal preparations) is no longer operative. Further evaluation should help provide an answer.
==============================
P.S. — for "Purists": As a longterm "student of French" — I have wondered for decades what the "correct" spelling for TdP is. French grammar is beautiful and challenging — and I have seen numerous versions in anglo texts regarding the spelling of this fascinating arrhythmia.
- First described by the French physician, François Dessertenne in 1966 — the French version of Wikipedia allows for 2 potential spellings: i) Torsades de Pointes; and, ii) Torsades de Pointe.
- The English version of Wikipedia adds: iii) Torsade de Pointes and, iv) Torsades des Pointes.
It does gets confusing ... So I contacted Dr. Pierre Taboulet (French cardiologist with special expertise in the intricacies of ECG interpretation — and creator of the wonderful e-cardiogram ECG Blog — that I highly recommend for French-speaking clinicians).
- Dr. Taboulet acknowledges that even French-speaking clinicians use different terms for TdP. That said, in his words — it really is much simpler than it may seem because — "Il y a une "torsade de(s) pointes", ce qui est le phénomène de base — mais quand il y en a plusieurs (ce qui en est presque toujours le cas), il y a des "torsades de pointes"!
- Loosely TRANSLATED — The basic phenomenon regarding TdP is that there is one episode of a "twist" (around the baseline) of the QRS tip (or point) — but if a given patient has several runs of TdP (which is almost always the case) — then there will be multiple episodes with "twist(s)" (around the baseline) of the points (the ups & downs of the QRS).
- My sincere THANKS to Dr. Taboulet for explaining this concept that I've wondered about for decades. His explanation strengthens my preference to continue uniformly using "Torsades de Pointes" as the written form of TdP. But the reality is that clinicians around the world (and in the literature) will continue to use multiple other spellings.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.