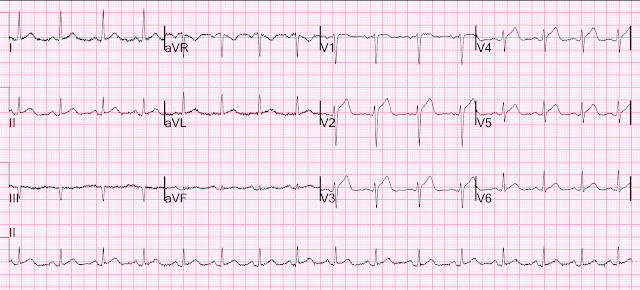
This ECG was texted to me with no other information. I assumed the presentation was consistent with acute MI.
What did I say?
"OMI. Activate the cath lab."
The T-waves in V2-V6 are diagnostic. It does, in fact, the STE meets STEMI criteria since there is 1 mm of in V4 and V5.
There is also some non-diagnostic STE in inferior leads. There is zero reciprocal ST depression. 50% of LAD OMI have zero reciprocal ST depression!
But it looks a lot like normal variant STE (also known as "early repolarization".
Then I sent it to the Queen of Hearts PMCardio AI Bot and she gave this response:
I also later used the 4 variable formula:
19.6 is all but diagnostic of LAD occlusion.
In spite of a relatively short QTc of 376 ms, the very low R-wave amplitude in V4 and the ST Elevation at 60 ms after the J-point in lead V3 contribute to a high final value.
Here is the clinical story:
A 40 year old male with no cardiac history presented with acute substernal chest pain that started 40 minutes prior to arrival. He had been having similar episodes for the past week, lasting no more than 5 minutes. He reported associated diaphoresis, radiation to the bilateral upper extremities and mild shortness of breath.
The first ECG was recorded at 53 minutes after pain onset.
He was given NTG sublingual.
The pain began to improve and this ECG was recorded:
Then the pain completely resolved and another ECG was recorded:
--Ruptured plaque in the distal LAD
--Diffuse coronary artery disease is noted in LAD branch vessels and a small LPL branch
--LAD is a large-caliber vessel that wraps around the apex (this explains the STE in inferior leads)
--First diagonal branch is a medium caliber with diffuse severe stenosis in the medial branch
--There is diffuse 40% stenosis in the proximal and mid LAD
--D2 is a small to medium caliber with tandem 70% stenoses in the ostial/proximal segment
--There is a hazy 95% stenosis in the distal LAD with angiographic characteristics of plaque rupture
--Apical LAD flow is TIMI-3 on initial angiography
It is important to remember that 20% of definite STEMI (OMI that everyone agrees are STEMI) have TIMI-3 (perfect) flow at angiography. And you can see why: the artery may sponstaneously reperfuse, as it did here well before angiography, and documented with resolution of pain and evolution of the ECG to typical full reperfusion pattern
Peak troponin I was 8544 ng/L. This is typical for a brief LAD OMI.
In some of our studies, this ECG would be classified as a false positive because the TIMI flow was perfect and the peak troponin was not over 10,000 ng/L!
Formal echo:
--Normal left ventricular size, mildly increased wall thickness, and normal function.
--Estimated left ventricular ejection fraction 55-60%.
--Regional wall motion abnormality--mid to apical anterior, mid anteroseptal, and apical septal akinesis.
MY Comment, by KEN GRAUER, MD (9/22/2023):
===================================
- How can we know that this ECG should not be mistaken for a repolarization variant?
- Which 1 or 2 leads are KEY?
-USE%20copy.png) |
| Figure-1: I've labeled the initial ECG in today's case. |
- What lowered my confidence in calling ECG #1 a definite OMI — was the finding of somewhat similar-appearing, upright T waves with slight-but-real J-point ST elevation in so many leads (ie, leads I,II,aVF; V2-thru-V6).
- My confidence was also lowered by the complete lack of any ST elevation or depression in lead aVL (which is usually my "Go To" lead when looking for confirmation of acute inferior OMI, or for acute LAD occlusion).
- Unless the ECG in Figure-1 was obtained as "routine" in an absolutely asymptomatic patient (or unless a prior tracing on this patient could be found showing identical ST-T wave morphology) — the 2 leads enclosed within the dotted BLUE rectangles ( = leads V4 and V5) — simply can not be interpreted as "normal".
- Instead — leads V4 and V5 have to be interpreted as having hyperacute T waves that are clearly disproportionate to their respective QRS (ie, These T waves are taller in size — "fatter"-at-their-peak — and wider-at-their-base than expected, given the small R wave amplitude in these leads).
- Once I identified leads V4 and V5 as definitely abnormal — I looked closer at neighboring leads. Looking more laterally, while the R wave in lead V6 was clearly taller than the T wave in this lead — in the context of knowing that leads V4,V5 were hyperacute — the T wave in lead V6 looked "fatter"-than-expected — and the base of this T wave was clearly widened.
- Looking more proximally (in the context of knowing leads V4 and V5 were hyperacute) — lead V3 (and by extension, probably also lead V2) manifest a taller-than-expected and wider base than is generally seen with repolarization variants.
- MY Impression Thus Far: Learning what the history in today's patient is — was clearly critical to optimal interpretation. That said — IF there was any history of recent symptoms, my interpretation would be multiple hyperacute chest lead T waves until proven otherwise.
- As noted above — I was surprised by lack of any ST segment deviation in lead aVL. That said —
- The Qr pattern in lead III (BLUE arrow) — was clearly abnormal! Although the finding of an isolated Q wave in lead III is by itself not necessarily abnormal — this Q wave was much larger and wider, as well as followed by a small-but-definite terminal positive deflection (r') — which generally is not seen as a normal finding in lead III.
- In support of this Q wave in lead III being abnormal — is the small-but-definite q wave in lead II (within the dotted BLUE circle).
- Finally — I though lead aVF looked extremely suspicious! (ie, with a straightened ST segment takeoff — and considering tiny size of the R wave in this lead, a hyperacute-looking T wave).
- P.S.: While by itself, the ST-T wave in lead I would not necessarily look abnormal — there is J-point ST elevation in this lead, that in the context of all of the other findings may well be part of the acute picture.
- As discussed above in Dr. Smith's excellent discussion — serial ECGs, correlated to severity of patient symptoms soon confirmed the acute event in today's patient.






No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.