Submitted by Van Wall M.D., Written by Pendell Meyers
Let's go back to the basics for a common and classic scenario.
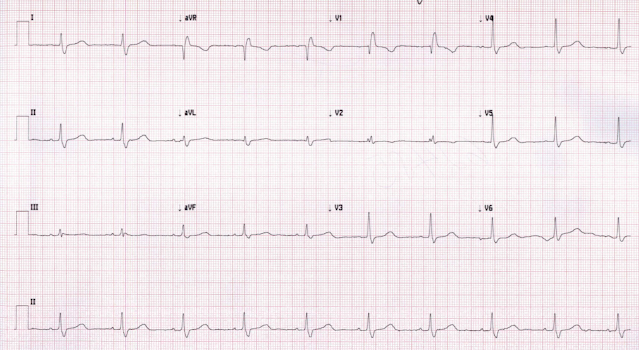
A middle-aged patient presents with shortness of breath and palpitations. The patient was stable without signs of low cardiac output or distress. Her ECG is shown below (first see what you think without using the baseline):
 |
| What do you think? |
There is a (minimally) wide complex, regular monomorphic tachycardia at a little faster than 150 bpm. I measure the QRS duration at almost exactly 120 ms. The differential would include ventricular tachycardia, any cause of narrow complex regular tachycardia plus added conduction aberrancy (such as a bundle branch block), or other causes of QRS widening like hyperkalemia or sodium channel blockade. Of course, the interpreter should always start by assuming that a wide complex monomorphic tachycardia is due to ventricular tachycardia and/or life threatening hyperkalemia, until proven otherwise.
This demonstrates why it is so important to be able to recognize RBBB, LBBB, and paced rhythms (pacer spikes) so quickly. This ECG has perfect RBBB morphology, one of the rare times that we can be confident that a regular wide complex rhythm is not classic ventricular tachycardia.
For more discussion on features of SVT vs. VT, see these prior posts:
A prior baseline showing identical RBBB morphology during sinus rhythm would prove this definitively.
Here is the prior baseline ECG on file:
They applied Lewis leads to see if they could get a better look at the atrial rhythm:
They gave 12 mg adenosine (a perfectly reasonable and guideline-endorsed option for any rhythm that is regular and monomorphic, regardless of QRS width):
Here is the prior baseline ECG on file:
 |
| This shows the same RBBB morphology in sinus rhythm. |
They applied Lewis leads to see if they could get a better look at the atrial rhythm:
 |
| I can't say that I see clear atrial activity. |
Flutter waves are revealed.
The rhythm soon returned to 2:1 atrial flutter, of course. The patient was then rate controlled and did well.
Learning Points:
Assume that wide complex regular tachycardia is VT and/or hyperkalemia. Then work backwards and prove that assumption false, if possible. VT is more likely statistically, and the likelihood of VT increases further with age, cardiac pathology, and QRS duration.
Recognizing classic RBBB or LBBB morphology may enable the diagnosis of SVT with aberrancy. This can be basically definite if the morphology is shown to be identical to prior known RBBB or LBBB morphology on baseline ECG.
Adenosine is contraindicated in irregular or polymorphic QRS complex rhythms. It is not contraindicated for wide complex regular monomorphic tachycardia, and is very reasonable in this scenario.


Great case, I must say. It was easy to identify the RBBB morphology but I must say that I struggle to see the "flutter waves" following adminstration of adenosine. The atrial activity looks more chaotic than fluttery.
ReplyDeleteAny tips on how to better identify them?
I think in lead 2 rhythm strip I can convince myself I see a faint regular undulation that happens at 300 msec intervals. But you're right: if this is truly flutter waves, it is certainly very very subtle. I should have explained that better, thanks for the comment. There is a chance I'm wrong, and it was instead SVT, however Dr. Wall tells me that the rhythm soon returned and required longer term rate control, and ECGs after rate control indeed confirmed Atrial Flutter. But you're right that we could not be certain of flutter waves from just the ECG above. Thanks!
DeleteIs it atypical flutter? Can’t see typical saw-tooth pattern even after adenosine..
ReplyDeletesee comment above. I agree it is not typical, very subtle.
Deletevery cool, Dr Van Wall, and Pendell... i think actually (like for the first time in three years!) got this one correct at the first ecg.. and decided adenosine was a reasonable trial.
ReplyDeletevery cool discussion. thanks to you both.
Dr. Pendell, Excellant teaching ECG with crisp discussion and learning points. May I add one more
ReplyDeletelearning point ? Whenever we have regular tachycardia at a rate of about 150/mt, with invisible
P waves, assume Atrial Flutter with 2:1 AV response. In the Lewis lead ECG, flutter waves are
visible one each between two QRS complexes. Now applying Harold Bix rule, it amounts to Atrial
Flutter @ 300/mt with 2:1 AV response. With regards, Dr.R.Balasubramanian. Pondicherry - INDIA
thanks very much!
Delete