An 82 yo male stopped for lunch after cycling. Witnesses reported a syncopal episode lasting approximately 30 seconds. He has a history of prior MI with 3 stents placed. There was no other significant hx.
The patient denied any chest discomfort, dyspnea, or n/v or any complaints and did not wish to go to the hospital. However, he did not protest transport.
BP was 134/66, and heart rate remained around 60, which he said was normal for him.
A 12-lead ECG was recorded:
The medic is very good at recording serial ECGs, and did so this time at 9 minutes even though there were no new symptoms (patient asymptomatic).
The ECG does not, strictly speaking, meet STEMI criteria: note on the side there are measurements of ST elevation at the J-point: it is correctly reading more than 1 mm ST elevation in 2 leads (II and V5), but these are not consecutive leads. STEMI criteria require the findings to be present in at least 2 consecutive leads.
The medic was now very worried in spite of absence of symptoms, and recorded another ECG 6 minutes later:
The medic noticed these dynamic findings and activated the cath lab!
They were headed to a non-PCI center, so activating meant activating a transfer. But they were too close to bypass the smaller hospital, so they stopped and the patient had an immediate ECG in the ED, still with no symptoms!!:
The patient was immediately transported to the PCI hospital, where an ostial RCA 95% thrombotic occlusion was found and opened and stented.
Comment
Should we get serial ECGs on asymptomatic syncope patients? Maybe. The literature on serial ECGs, which is pretty old, would say that among patients who are unlikely to have ACS, or at least dynamic ACS, it takes more resources than it is worth. One should clearly get serial ECGs on a patient with ongoing chest pain, but for a single episode of syncope without ongoing symptoms?
But in the ambulance, the ECG leads may remain attached, so why not record multiple tracings?
In contrast, in the ED, there is much demand for the ECG machine and tech, and it is more use of resources to keep the machine attached and record multiple tracings, so I would not advocate for that.
Learning Points
1. If it does not strain resources, record serial ECGs whenever there is any suspicion for ACS.
In this case, suspicion was very low but the medic is an incredibly skilled ECG reader (I know him) and he noticed these slight abnormalities which made him record more and then activate the cath lab.
2. In this case, the computer was very sensitive for STEMI.
The patient denied any chest discomfort, dyspnea, or n/v or any complaints and did not wish to go to the hospital. However, he did not protest transport.
BP was 134/66, and heart rate remained around 60, which he said was normal for him.
A 12-lead ECG was recorded:
The medic is very good at recording serial ECGs, and did so this time at 9 minutes even though there were no new symptoms (patient asymptomatic).
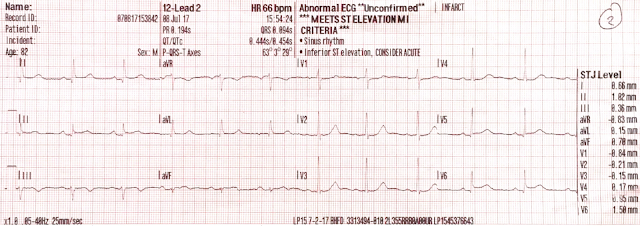 |
| Sinus rhythm. Note there is new ST elevation in lead II, aVF, V5, and V6. There is also increased sagging of the ST segment in V1-V3. The computer surprisingly reads "Meets STEMI critiera" !! |
The ECG does not, strictly speaking, meet STEMI criteria: note on the side there are measurements of ST elevation at the J-point: it is correctly reading more than 1 mm ST elevation in 2 leads (II and V5), but these are not consecutive leads. STEMI criteria require the findings to be present in at least 2 consecutive leads.
The medic was now very worried in spite of absence of symptoms, and recorded another ECG 6 minutes later:
 |
| Now the T-wave in lead III is much less negative. There appears to be LESS ST elevation in II, V5, and V6 |
The medic noticed these dynamic findings and activated the cath lab!
They were headed to a non-PCI center, so activating meant activating a transfer. But they were too close to bypass the smaller hospital, so they stopped and the patient had an immediate ECG in the ED, still with no symptoms!!:
 |
| Atrial flutter with slow and variable conduction Obvious inferior - posterior - lateral STEMI Note that inferior T-waves have "pseudonormalized" (become upright) See here for more on pseudonormalization |
The patient was immediately transported to the PCI hospital, where an ostial RCA 95% thrombotic occlusion was found and opened and stented.
Comment
Should we get serial ECGs on asymptomatic syncope patients? Maybe. The literature on serial ECGs, which is pretty old, would say that among patients who are unlikely to have ACS, or at least dynamic ACS, it takes more resources than it is worth. One should clearly get serial ECGs on a patient with ongoing chest pain, but for a single episode of syncope without ongoing symptoms?
But in the ambulance, the ECG leads may remain attached, so why not record multiple tracings?
In contrast, in the ED, there is much demand for the ECG machine and tech, and it is more use of resources to keep the machine attached and record multiple tracings, so I would not advocate for that.
Learning Points
1. If it does not strain resources, record serial ECGs whenever there is any suspicion for ACS.
In this case, suspicion was very low but the medic is an incredibly skilled ECG reader (I know him) and he noticed these slight abnormalities which made him record more and then activate the cath lab.
2. In this case, the computer was very sensitive for STEMI.


Thanks Steve for this new post.
ReplyDeleteOn the first ECG :
- flat T wave in lead II
- subtle up-down T wave in lead III "towers" microQRS
- are QRS fragmentation in leads II, III, aVF specific for coronary artery disease even without LBBB ?
Great observations. I don't think the "fragmented QRS" is meaningful, but your other observations are very keen and probably represent early ischemia.
DeleteI don't seem to understand this one. So, when I see inverted t's I consider ischemia, look for the possibility of it being reperfusion t waves, or just benign. But the T wave becoming less negative in lead III is what made this EKG suspicious for occlusion? This is a tough one to grasp.
ReplyDeleteShanen, this is what happens in pseudonormalization. With reperfusion, T-waves invert. With re-occlusion, they become less negative and then become upright. Look at all these cases of pseudonormalization: http://hqmeded-ecg.blogspot.com/search?q=pseudonormalization
DeleteIs there any protocol about how "serial ECG's" are done? How frequent, and how many?
ReplyDeleteKind regards,
Maarten Van Hemelen
IM resident
Maarten,
DeleteI do them every 15 minutes for at least an hour.
STeve
Nice case, with credit to that medic for picking up on subtle ECG findings. I’d add the following thoughts. Reasons why the 1st ECG is definitely not normal include in addition the appearance of lead V2 — which shows clearly abnormal early transition (with a predominant R wave). In the context of an elderly patient with syncope — the T wave in this lead looks taller and broader-than-it-should be. The shape of the ST segment in lead aVF, though tiny in amplitude — is coved. In that context, the T inversion in lead III looks deeper than expected for a simple T wave following QRS vector change. And while lead II doesn’t show ST-T inversion/depression — the ST segment in this lead is flat, yet not flat in any other of the 11 leads. All of changes are admittedly VERY subtle and nonspecific, with the additional problem of not having a prior ECG on this patient with a history of a prior MI — but taken together in the context of an older patient with symptoms that may relate to an acute/recent event — this IS a suspicious tracing that is possibly indicative of something acute and evolving in need of close follow-up. Again — excellent case!
ReplyDeleteThanks, Ken.
Delete>> it is correctly reading more than 1 mm ST elevation in 2 leads (II and V5), but these are not consecutive leads.
ReplyDeleteIt is correctly reading 1 mm ST elevation in V5 and V6.
Dear colleagues
ReplyDeleteAccordingly with new classification of affected walls the MI should be reported as inferobasal/lateral STEMI
BAYES DE LUNAet al demonstrated with cardioMRI that the dogma of posterior wall cannot be accepted and that tall R in v1+ elevation ST in v5/6 should be reported as lateral instead of posterior. Isn't? Although I am concerned about the message of this magnific case...
Thanks
Bayes de Luna's demonstration is academic in the EKG world. There clearly is a difference between inferobasal infarction (with ST depression in right precordial leads) and lateral infarction. I find his classification does harm to EKG analysis and is not relevant.
DeleteDear Dr Smith : I must apologize for my limited knowledge compared to yours. I am only a family doctor interested in ecg. I found your case very very excelent for first med contact in ACS chain code. Nevertheless when you comment:"infero-posterior- lateral stemi" must we accept that posterior wall exists?
ReplyDeleteI read a few years ago that just posterior wall is not demonstrated...Thank you very much and congratulations
Just look a the map of segments (links below). You can see that segment 5 is posterior, no matter what Bayes de Luna wants to call it. And it is very distinct on the ECG: when there is transmural ischemia, leads on the back (Posterior) show ST elevation and the (anterior) right precordial leads show reciprocal ST depression.
Deletehttps://www.barnardhealth.us/echocardiography/images/2154_51_114-aha-segment-model.jpg
http://www.annals.in/articles/2013/16/4/images/AnnCardAnaesth_2013_16_4_268_119175_f28.jpg