A young otherwise healthy man presented with 4 hours of sharp 10/10 substernal chest pain. It has been constant since then. He looked ill and diaphoretic. BP was 160.
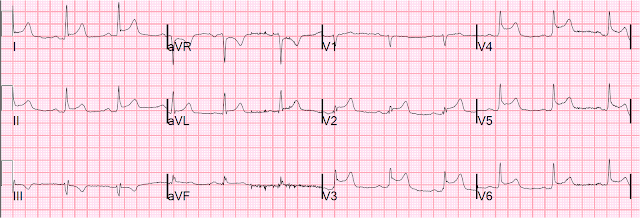
Here is his ECG at t = 0:
This ECG is diagnostic of anterior STEMI. And the Cath lab was activated immediately.
But there was some doubt as to whether it might be pericarditis because of the ST elevation in I and II, without ST depression in III. Add that to "sharp" pain and a 33 year old, and it is easy to convince yourself that this is, indeed, pericarditis.
However, look closely!
1. There is a fragmented QRS in lead V2 (potential goes up, then down, then up again). This is a good sign for myocardial infarction and does not happen in pericarditis.
2. The voltage in V2 is very small. This is a sign of MI, either acute or old.
3. There is terminal QRS distortion in V2 and V3 (you might dispute that V3 has what looks like a J-wave, but I would argue this is not what a true J-wave looks like)
After nitroglycerine, his systolic BP was 120 and his pain was improving. Heparin and aspirin were given. Another ECG was recorded at t = 27 minutes:
The patient went to the cath lab and had an 80% occluded mid LAD with fresh thrombus. It was a "type III" LAD, meaning it wraps around to the inferior wall. The distal inferior apical LAD was cut off by distal embolization from LAD culprit. The Right Posterior Descending Artery off the RCA was small, so that the RCA did not adequately supply the inferior wall.
Thanks to spontaneous reperfusion (helped by aspirin and nitroglycerin), the artery was open and the peak Troponin I only 12.2ng/mL.
Echo showed an apical, but not inferior, wall motion abnormality. This is likely because 1) the ischemia to the inferior wall was only partial and 2) it reperfused quickly.
Lessons:
1. Occlusion of a Type III (wraparound) LAD that supplies both the anterior and inferior wall can have "widespread ST elevation" that can be confused with pericarditis.
2. The QRS is at least as important as the ST segment in diagnosing STEMI
Here is his ECG at t = 0:
 | |
|
This ECG is diagnostic of anterior STEMI. And the Cath lab was activated immediately.
But there was some doubt as to whether it might be pericarditis because of the ST elevation in I and II, without ST depression in III. Add that to "sharp" pain and a 33 year old, and it is easy to convince yourself that this is, indeed, pericarditis.
However, look closely!
1. There is a fragmented QRS in lead V2 (potential goes up, then down, then up again). This is a good sign for myocardial infarction and does not happen in pericarditis.
2. The voltage in V2 is very small. This is a sign of MI, either acute or old.
3. There is terminal QRS distortion in V2 and V3 (you might dispute that V3 has what looks like a J-wave, but I would argue this is not what a true J-wave looks like)
After nitroglycerine, his systolic BP was 120 and his pain was improving. Heparin and aspirin were given. Another ECG was recorded at t = 27 minutes:
 | |
|
Thanks to spontaneous reperfusion (helped by aspirin and nitroglycerin), the artery was open and the peak Troponin I only 12.2ng/mL.
Echo showed an apical, but not inferior, wall motion abnormality. This is likely because 1) the ischemia to the inferior wall was only partial and 2) it reperfused quickly.
Lessons:
1. Occlusion of a Type III (wraparound) LAD that supplies both the anterior and inferior wall can have "widespread ST elevation" that can be confused with pericarditis.
2. The QRS is at least as important as the ST segment in diagnosing STEMI

Dr. Smith,
ReplyDeletethe frontal axis is normally towards lead II (60 degrees) in pericarditis...
In this case, it is closer to lead I (looks to be about 15 degrees).
This case seems clear without considering axis, but generally does the axis factor into your analysis of STEMI vs pericarditis?
DaveB
Dave,
DeleteYou're absolutely right. The ST axis in pericarditis is usually towards lead II, so this is a bit abnormal for pericarditis. But it is also abnormal for STEMI. Anterior STEMI ST axis is anterior, unless it is proximal LAD occlusion, in which case it is anterior and superolateral (with ST depression in II, III, aVF). Diagonal occlusion can have "mid anterolateral" ST elevation, which is in I, aVL, and V2 (anterior and superior). But to have it directly towards V2 and I (ST axis 0) is also not common.
Steve
Hi Dr Smith,
ReplyDeleteWe had a recent similar case (prehospitally) where the Cath lab upon global ST elevation - pt had a wrap-around LAD. I am trying to find current information on the % population with this type of LAD with little success. Would you have any information pertaining to this?
Cheers, Dachs
Dachs,
DeleteI have seen many of these cases. See the label "wraparound LAD" for more of them. However, I have had little success in finding literature on it. It must exist. If you find some, let me know.
Steve Smith
Dr. Smith,
ReplyDeleteThis may be related to your answer to Dave's question. I understand how we see the STE in II, due to the 'wraparound' variant identified on Cath. But how can we understand the 'high lateral' lead STE (I, aVL) with a mid-LAD lesion? Looking at the ECG, I would have expected a more proximal lesion. (I believe you have a different case on your blog where you indeed prompted a re-reading of the cath based on the ECG findings that didn't match the lesion blamed - why is this not one of those cases?). Thanks!
~Nick
Nick,
DeleteVery good question and I don't know the answer. I haven't seen the angiogram. There is probably some anatomical explanation on it.
thanks,
Steve Smith
Great discussion - I published a similar case with a twist this week at http://underneathEM.com/2012/08/not-all-st-elevation-is-stemi/ and followed up at http://underneathEM.com/2012/08/not-all-st-elevation-is-stemi-the-follow-up/ but I particularly like your comments about QRS amplitude and morphology, especially with regard to V2. These are by relevant to the ECG I discussed. Thanks Steve!!!
DeleteDr Smith,
ReplyDeleteI really enjoy your post.
Could we say that there is no PR elevation in aVR, hence pericarditis is less likely ? So as there is ST depression in aVR that support the diagnosis of Ant-inf STEMI ? Thanks
Malsia
That's a good point, but there might be a bit of PR elevation in aVR (and PR depression in some other leads), but that is because this can be a normal finding of normal atrial repolarization. See this post: http://hqmeded-ecg.blogspot.com/search/label/atrial%20repolarization%20wave
DeleteNice one
ReplyDeleteDr. Smith,
ReplyDeleteJust wondering if you could provide the literature that demonstrates fragmented QRS's do not occur in pericarditis? I'm finding in the literature that while a fragmented QRS is associated with ischemic heart disease--it's not particularly specific and is also a marker of infiltrative cardiac disease, LVH, etc. etc. which might also be present in a patient with acute or even post-MI pericarditis. Thank you!
I am unaware of literature on this, but fragmented QRS, as you say, is a marker of myocardial disease. In a previously healthy patient, what is the most likely myocardial disease when there is ST elevation? It is infarct. Is it possible that this is due to something else? Of course. Would pericarditis do this? No - it is not a myocardial disease. Would myocarditis do this? Maybe, but I have never seen a report of it. Perhaps you have? The chances that this is due to something other than MI are vanishingly small. Do you want to bet the patient's life on it?
ReplyDeleteSteve Smith
Do we need 2 contiguous leads to call it fragmented qrs ??
ReplyDeleteNo. There are times when you might question if notching in the QRS is the result of "scar" (ie, from prior infarction or cardiomyopathy) — for example, one normally expects a triphasic rSR' complex in lead V1 with RBBB. So the "right clinical context" — the more leads you see unexpected notching (fragmentation) in — and the overall "look" of the ECG are all factors that I use together to decide if I think there is "fragmentation" — :)
ReplyDeleteTks Ken.
ReplyDeleteThe Aug 5 2018 post where fragmented qrs is defined, prompted me to ask that..
@ AKS — Understood! I suspect the concept of "fragmentation" is one in which different electrocardiographers may assess somewhat differently. Using the combination of factors I noted in my earlier reply are what are most helpful to me — :)
DeleteOkay - :)
ReplyDelete