This was sent to me by a reader who wishes to remain anonymous.
A lady in her 60s came to the ER with chest discomfort and shortness of breath. She had a history of previous anterior MI treated by primary PCI to the proximal LAD. The first EKG is from 2:30 PM on the day of presentation to the ER.
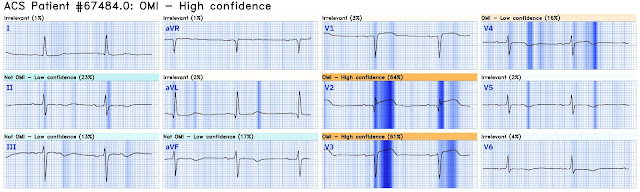
Smith: To me this is a blatantly obvious acute anterior OMI. There are massive hyperacute T-waves in V2 and V3. There is ST Elevation that does not meet criteria in V2 and V3. My eyes would bulge within a second of viewing this ECG.
I texted this to our group "EKG Nerdz," asking "Do you think that anyone could miss this?"
Pendell answered: "Sounds like a story that happened at least several other times today but nobody texted you about it." (i.e, yes, they could miss it)
Willy Frick answered: "Obvious as an OMI. Subtle as a STEMI." (i.e., you MUST know the OMI paradigm in order to "see" this ECG)
Here is the Queen of Hearts interpretation:
Click here to sign up for Queen of Hearts Access
Here is the cardiologist's formal interpretation: "sinus rhythm with marked sinus arrhythmia, left ventricular hypertrophy with repolarization abnormality, and anteroseptal infarct, age undetermined." This terrible ACUTE anterior total infarct is not recognized by a cardiologist.
When initial troponin I returned at 158 ng/L, she was diagnosed with NSTEMI. The patient was admitted for observation. No repeat ECG was recorded.
It is widely believed that hyperacute T-waves are a transitional state preceding ST Elevation1–4 Thus, it is tempting to postulate that early cases of OMI will eventually evolve to STEMI; yet, our data contradicts that notion. In our study, there were 20/53 complete LAD OMI (TIMI-0 flow) which did not meet STEMI criteria. All were diagnosed on the first ECG by both the expert (Smith) and the Queen of Hearts. 17/20 patients with acute complete LAD occlusion without STE had hyperacute T-waves on their initial ECG; 16/20 had subsequent ECG(s) recorded. None of the 20 ever evolved to STEMI criteria.
1. Koechlin L, Strebel I, Zimmermann T, Nestelberger T, Walter J, Lopez-Ayala P, Boeddinghaus J, Shrestha S, Arslani K, Stefanelli S, Reuthebuch B, Wussler D, Ratmann PD, Christ M, Badertscher P, Wildi K, Giménez MR, Gualandro DM, Miró Ò, Fuenzalida C, Martin-Sanchez FJ, Kawecki D, Bürgler F, Keller DI, Abächerli R, Reuthebuch O, Eckstein FS, Twerenbold R, Reichlin T, Mueller C, APACE investigators. Hyperacute T Wave in the Early Diagnosis of Acute Myocardial Infarction. Ann Emerg Med [Internet]. 2023;82:194–202. Available from: http://dx.doi.org/10.1016/j.annemergmed.2022.12.003
2. Zorzi A, Perazzolo Marra M, Migliore F, Tarantini G, Iliceto S, Corrado D. Interpretation of acute myocardial infarction with persistent “hyperacute T waves” by cardiac magnetic resonance. European Heart Journal: Acute Cardiovascular Care [Internet]. 2012;1:344–348. Available from: https://journals.sagepub.com/doi/abs/10.1177/2048872612466537
3. Verouden NJ, Koch KT, Peters RJ, Henriques JP, Baan J, van der Schaaf RJ, Vis MM, Tijssen JG, Piek JJ, Wellens HJ, Wilde AA, de Winter RJ. Persistent precordial “hyper acute” T-waves signify proximal LAD artery occlusion. Heart [Internet]. 2009;Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19620137
4. Dressler W, Roesler H. High T waves in the earliest stage of myocardial infarction. Am Heart J [Internet]. 1947;34:627–645. Available from: https://www.sciencedirect.com/science/article/pii/0002870347903438
MY Comment, by KEN GRAUER, MD (10/8/2024):
- For clarity in Figure-1 — I’ve labeled today’s initial tracing. I interpreted this tracing knowing only that the patient was a woman in her 60s, with a prior history of proximal LAD OMI — who now presented to the ED with a history of new chest discomfort and shortness of breath.
-labeled-USE.png) |
| Figure-1: I've labeled the initial ECG in today's case. (Digitized using PMcardio to improve visualization). |
- KEY Point: The important distinction that has to be made in today's case, is between ECG findings consistent with this patient's prior LAD OMI — vs — ECG findings of a new acute event superimposed on these prior ECG findings.
- QS complexes are seen in each of these first 3 anterior leads — with marked fragmentation of the QS complex in lead V3. Clearly, this patient has had anteroseptal infarction at some point in time.
- Although the shape of the ST elevation is abnormal in the first 2 anterior leads (coved in lead V1 — with straightening of the ST segment takeoff in lead V2) — the amount of actual ST elevation is relatively modest (although probably still excessive in lead V2 — considering the very small amplitude of the QS complex in this lead).
- The above said — there should be no doubt that the amount of J-point ST elevation in lead V3 is excessive, in association with a hypervoluminous hyperacute appearance of the ST-T wave in this lead that is large enough to "swallow up" the small, fragmented QS in V3.
- In the context of this woman in her 60s who has known coronary disease (and who is now presenting with acute chest discomfort) — I interpreted neighboring leads V1 and V2 as part of the same acute process suggested by the QRST in lead V3. And in association with the flattened ST depression in lateral lead V6 (and to a lesser extent in lead V5) — my ECG impression was precordial "Swirl", indicative of acute proximal LAD occlusion superimposed on prior infarction — until proven otherwise. (For more on Precordial Swirl — See the October 15, 2022 post in Dr. Smith's ECG Blog).
- In support of my impression that the ST-T wave changes in the chest leads are acute until proven otherwise — is the ST segment flattening and depression in lead II — as well as the J-point ST depression in lead I (BLUE arrows in these leads).
- Prompt cath to define the anatomy should be expedited.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.