Below are ECGs from six different patients. All of the patients contacted EMS due to acute onset chest pain. Imagine you get these ECGs in real time and you are asked whether or not the cath lab should be activated? All ECGs in this case have saddleback ST elevation. Which of the ECGs represent OMI?
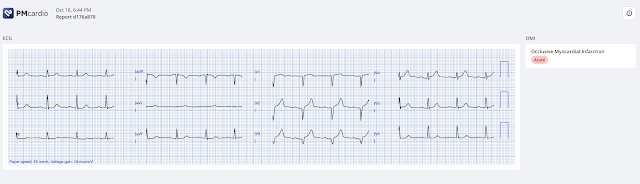
ECG #1
Case 1. The above ECG is from a 70 something male with chest pain. The ECG was originally recorded at 50mm/s paper speed. It has been compressed on the X-axis so it looks like it was recorded at 25mm/s. What do you think?
ECG #2
Case 2: The above ECG was obtained from a diabetic 45 year old smoker with chest pain. What do you think of the ECG changes here?
ECG #3
Case 3. This ECG (above) was recorded from a 55 year old male patient with acute onset chest pain and diaphoresis. How would you interpret this ECG?
ECG #4
Case 4: The above ECG belongs to an 80 something male with acute onset chest pain radiating to the back. How would you assess the ECG changes here?
ECG #5
ECG #6
Discussion: When a patient presents with chest pain and ST segment elevation we need to evaluate whether or not the ST elevation is ischemic in nature. The ST-segment and beginning of the T-wave in a non-ischemic ECG usually have a slightly upward concave appearance. Ischemia often produces a straightening of the ST segment and sometimes upward convexity. Saddleback ST segments are usually not ischemic in origin, but as with all other «rules», there are exceptions. In today’s post we have shown six ECGs out of which three were OMI and three were not.
Case #1 OMI, Queen gets it right
The ECG shows sinus rhythm with a narrow complex QRS. There is ST elevation with saddleback morphology in the inferior leads (II, III and aVF). The inferior leads do not have a distinct J-wave. The T waves are bulky and appear hyperacute. Moreover the high lateral leads aVL, and I both show reciprocal discordant ST depression and T wave inversions. When looking at the precordial leads there is appreciable slight ST depression in lead V2 and inappropriately isoelectric ST segment i lead V3. All of these findings together makes this ECG diagnostic of inferior and posterior occlusion myocardial infarction (OMI)
The patient is this case was treated as if he had an ongoing OMI. Primary PCI was not feasible and therefore the patient was given thrombolytics by EMS. He arrived in our ED with the below ECG pain free. As you can see the ECG has changed dramatically with the thrombolytic therapy. There is now reperfusion of the artery.
Post thrombolytics ECG
As you can appreciate, the ST elevation in the inferior leads is gone. There is still hyperacute looking T waves in the inferior leads and ST depression V2-V4. Following the improvement in the ECG the patient's pain too improved drastically. This of course proves that the initial ECG was OMI and that the artery has reperfused. At cath later the same day, a proximal 99% RCA culprit lesion was stented. Troponin T peaked at 4051 ng/L. (ref < 14ng/L)
If the ECG after thrombolytics shows normalization of the ST segment and T wave changes and the patient is pain free, there is no need for urgent CAG. It is reasonable to wait a few hours after lytics if you are sure that the artery is reperfused. The GRACIA-2 trial showed that PCI is safe 3-12 hours after thrombolysis. Of course, the reperfused artery can re-occlude at any time, so these patients need to be on ST-guard and taken for immediate catheterization if they re-occlude. The QoH interpretation (below) was OMI with high confidence for ECG #1.
Case #2 FAKE (Mimic), Queen Version 2 gets it right
The second ECG in today’s case was obtained from a 45 year old male with a history of tobacco use. I was shown this ECG by a colleague who asked for my opinion. I said I thought it looked like a fake (in other words an OMI mimic). I sent this ECG to the EKG Nerdz group. You can see some of the answers below.

The patient ruled out with serial troponins being negative. Echocardiography was without wall motion abnormality. A previous ECG was later obtained that showed similar findings. ECG #2 does have ST depression and an inverted T wave in lead aVL just as in the first ECG in today’s case. Why is this reciprocal ST depression not suggestive of ischemia you may ask?. The ST segment and T wave in lead aVL are concordant to the QRS complex. This is a significant difference and the T wave inversion seen in aVL therefore cannot be given the same significance as in the first case in today's post. (See Dr. Smith comment below for more insight). Also there are no signs of posterior ischemia (ST depression) in leads V2-V4.
Smith: There is some reciprocal STD in aVL. Reciprocal STD in aVL is seen sometimes in non-ischemic ECGs, but is almost never seen in pericarditis (Bischof et al.). Moreover, the T-wave inversion in aVL is a normal finding because the QRST axis is normal; this means that the QRS axis and T-wave axis are close to each other. The QRS axis is approximately 110 degrees and the T-wave axis is approximately 80 degrees (this is best assessed by lead I, which has S-wave > R-wave (right axis deviation) but T-wave upright (more towards lead I than away from lead I). The difference is only 30 degrees and up to 45 degrees is normal. True "T-wave inversion" has a wide QRST angle.
The Queen of Hearts AI model version 1 interpreted ECG #2 as OMI high confidence. Version 2.0 (not yet released) was shown the exact same ECG and the interpretation was not OMI.
The image below shows that QoH version 1 interprets the ECG as OMI with high confidence (value close to 1 on the top line). Version 2 interprets the ECG as not OMI with high confidence (value close to 0 on the second line). It is remarkable how much the AI model has changed its interpretation of the same ECG. It now correctly and confidently identifies ECG #2 as not OMI
Case #3 OMI, Queen gets it right
This ECG shows sinus rhythm with a narrow QRS complex. There is an incomplete RBBB (rSr` in V1). There is left anterior hemi-block (QRS negative in lead II). Lead V2 shows saddleback ST-elevation. In leads V2-V5 there is ST elevation and (very impressive) hyperacute bulky T waves. In the inferior (II, III aVF) and lateral (I, aVL and V6) leads there are hyperacute T waves. This ECG is absolutely diagnostic of anterior and inferior OMI and is compatible with a wrap around LAD supplying the anterior and inferior wall.
Case #4 FAKE (Mimic) Queen gets it right
I was on call when I received this pre-hospital ECG. The patient is an 80 year old man with acute onset chest and back pain. The ECG shows significant ST elevation. I was somewhat concerned that the ECG represented OMI and activated the cath lab. The ECG shows qR complexes in leads V2-V3 with upward concave ST segment elevation. Saddleback ST elevation in V2 is rarely due to OMI. A much more common cause of saddleback ST elevation in V1-V3 is that the leads have been placed too high on the chest and this should always be checked. Here the P wave polarity in V1 and V2 are consistent with correct lead placement. (If V1 and V2 are placed too high, P waves are often of negative polarity in these leads)
I thought for a moment that the ECG might represent LVH, but I would expect slightly more (appropriately) discordant ST elevation in the inferior leads. I was concerned that the ECG represented some strange anterior OMI with inferior reciprocal isoelectric ST segments. I was not convinced that the ECG changes represented OMI, but I figured I had to prove it was not. It would be a terrible mistake to miss this as occlusion.
CAG showed significant LAD disease in the mid-segment. However, there was no thrombotic component and there was TIMI III flow in all coronaries and their main branches. In conclusion, CAG was interpreted as showing significant atherosclerotic disease, but it was not deemed likely to be causing the ECG changes. PCI was performed as the lesion was significant. The post-PCI ECG did not change. Troponin T drawn five hours after the onset of symptoms was 17ng/L. Troponin levels did not increase significantly. Below you can see the post PCI ECG and echo. A CT scan was done as part of the work up, but no definite cause of the patient's chest pain was identified.
- Thrombolytic therapy is recommended if primary PCI is not an option. Thrombolytics are more efficient the sooner they are given after symptoms onset.
- Thrombolytics will produce TIMI III flow in the culprit artery in just above 50% of the patients at 90 minutes.
- Most cases of saddleback ST elevation is not ischemic, but some are and it is our job as health care professionals to identify the patients with an occluded coronary artery
- Always consider (too high) lead placement as a cause of saddleback ST-E if present in leads V1-V2
MY Comment, by KEN GRAUER, MD (10/30/2024):
- Those of us used to some form of “objective competence testing” — probably approached today’s challenge in similar fashion as I did — that it is likely that some (but not all) of these 6 tracings represent acute OMIs in need of prompt cath — but a few don’t, and that there may be “equivocal findings" (to potentially throw us off) inserted along the way.
- My reason for suggesting this additional clinical approach to today’s ECG challenge is: i) All 6 of these ECGs show “saddleback” ST elevation and other remarkable ECG findings that need to be recognized; and, ii) The decision of “What to do?” — is not a “binary” one (ie, of OMI or no OMI ) — but rather includes a 3rd option of us not yet being able to exclude a potential acute OMI.
- It is “OK” — to not necessarily recognize all of the subtle acute findings that we highlight on Dr. Smith’s ECG Blog.
- It is “not OK” — not to recognize higher risk patients with abnormal initial ECGs that mandate immediate additional evaluation until such time that a definitive decision can be made regarding whether or not to activate the cath lab.
- Reminder: Even the experts will not always know with 100% certainty whether an initial ECG represents an acute OMI in progress. As a result — We need to remember the 3rd option, in which our goal is to identify patients for whom the initial ECG could be an acute OMI in progress — for whom we need to expedite additional evaluation to arrive at a definitive determination as fast as this is possible.
- The limb leads suggest an acute inferior STEMI — already with a large Q wave in lead III (hard to tell if there is a Q in aVF — or if this is an rsR' complex).
- The "magical" finding that we often emphasize of mirror-image opposite ST-T wave changes in leads III and aVL — confirms the diagnosis of acute inferior STEMI (reciprocal changes also being seen in lead I ).
- That the RCA is the "culprit" artery — is suggested by: i) ST elevation in III > II; — ii) Marked ST depression in aVL; and, iii) Lack of ST elevation in V6 (as might be expected with a LCx culprit).
- For me — 99+% certainty of OMI was attained by the associated presence of acute posterior OMI (ST flattening and depression in leads V2,V3).
- Despite inferior lead Q waves with ST elevation — I thought this was a "fake" because: i) The QRS in lead aVL is predominantly negative — so the relatively shallow T wave inversion is not necessarily abnormal (vs much deeper ST-T wave depression in lead aVL for ECG #1); — ii) Lead I suggests a right axis (which is far less common with simple inferior MI) — and there is no reciprocal change at all in lead I; — iii) There is no suggestion of posterior involvement; — and, iv) The ST-T waves in leads V3,V4,V5,V6 all look virtually the same as the ST-T waves in leads II,III,aVF — with V4,V5,V6 having a virtual identical appearance of leads II,III,aVF with Q wave and identical-looking ST-T elevation/peaking. In contrast — acute OMI usually localizes! (and is less likely to yield a near-identical QRST picture for 7/12 leads! ).
- Note that Drs. Nossen, Meyers, Smith and Frick all thought this was probably a "fake" — but that all of us emphasize less than 100% certainty based on this single ECG.
- That said — the important point is that a few simple actions are all that is needed for us to attain 100% certainty in a very short period of time (ie, finding a prior ECG on this patient for comparison — serial troponins — stat Echo — and repeating this ECG within 10-to-20 minutes).
- NOTE: This ECG #2 is not a normal tracing. Instead of acute OMI — I initially suspected acute myocarditis given the diffuse Q waves with ST elevation without localization. This would be a patient for whom I would want to find out WHY this non-OMI ECG looks so abnormal.
- This one was easy (ie, Took me less than 5 seconds) because: i) The history is classic ( = 55yo man with acute onset CP and diaphoresis); — ii) Not only are there giant-amplitude positive T waves (≥18 mm in V3,V4) — but these hyperacute T waves are extremely wide at their base; — iii) Counting the inferior leads — there are 9/12 leads with hyperacute T waves + anterior lead ST elevation + loss of R wave from lead V2-to-V3 + Incomplete RBBB with LAHB — which in this patient with new severe CP is 100% diagnostic of acute proximal LAD OMI.
- This case is a perfect example of a non-binary answer — in that while I did not think this ECG represented an acute OMI — I was not 100% certain (which is OK as long as we quickly rule out an acute event — which was done in this case by cardiac cath that showed significant LAD disease, but no acute OMI ).
- LVH is clearly present by voltage (markedly increased R waves in leads I,aVL and the overly deep S in lead III ) — with LV "strain" definitely seen in lead aVL, with a "strain equivalent" in lead I.
- The deep Q waves in leads V2,V3 are definitely abnormal, in association with marked ST elevation in these leads (and to a lesser extent in lead V4).
- That said — the overall picture to me did not "look" acute — and the history of "chest pain radiating to the back" in this 80-something man with marked LVH — made me strongly consider an aortic dissection as a more likely cause.
- Without a prior ECG for comparison — there would be no way to know IF the above ECG changes were new or old. And, even if there was acute aortic dissection — the dissection could result in occlusion of a coronary artery. As a result, even though I thought acute OMI as a primary event was less likely based on this single ECG — additional evaluation would be needed to confirm my impression. (Aortic dissection was apparently ruled out by a negative CT scan).
- This case illustrates another example of a non-binary answer — in that while I did not think this ECG represented an acute OMI — I was not 100% certain. As a result — additional evaluation was needed (which ruled out an acute event).
- i) The shape of the ST elevation manifests an upward concavity (ie, "smiley"-configuration).
- ii) As per Dr. Nossen — there is J-point notching in lead II — and a terminal "slur" in leads III and aVF (which as per My Comment in the October 15, 2024 and May 23, 2022 posts — often serves as a J-point notch "equivalent" sign of a repolarization variant, especially when associated with rapid upsloping of the ST segment).
- iii) An isolated Q wave in lead III (as we see here) — is not necessarily abnormal.
- iv) The very shallow T inversion in this lead aVL (in which the QRS is almost biphasic) — does not qualify as "reciprocal" ST depression.
- v) The QTc is not at all increased.
- vi) There is no sign of posterior OMI (ie, There is slight, gently upsloping J-point ST elevation in leads V2 and V3 — as should occur normally).
- vii) R wave progression is normal, with good R wave amplitude.
- This ECG is obviously abnormal because: i) There is ST depression in all 3 inferior leads (with a down-up biphasic T wave in III and aVF); — ii) There is ST elevation in lead aVL (with potentially a hyperacute T wave); — iii) There is ST elevation in leads V1 and V2 — with very tall, upright T waves in leads V2,V3,V4.
- IF the history had been "sudden onset of severe chest pain" — I would have instantly thought acute LAD OMI with need for prompt cath.
- That said — the history we were given says, "70-something male with vague pressure-like chest discomfort". No "onset" of symptoms is provided. As a result — this is a case for which I'd want to quickly gather more information to verify if despite only "vague" chest discomfort — an acute event was in progress. 'Sometimes ya just gotta be there!" — and it may be that a 2-second glance at the patient would have immediately conveyed acuity.
- In any event — the findings in ECG #6 are so striking that no more than minutes should be taken to order stat Troponins — repeat the ECG (and search for a prior tracing) — and do bedside Echo.

















-labeled-USE.png)