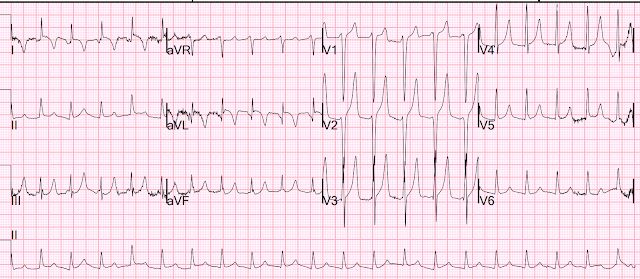
I was reading EKGs on the system and came across this one:
The K came back at 6.2 mEq/L.
The patient was treated.
He ruled out for MI by troponins.
No followup EKG was recorded!!
See many examples of Pseudo STEMI due to hyperkalemia at these two posts:
Acute respiratory distress: Correct interpretation of the initial and serial ECG findings, with aggressive management, might have saved his life.
- As always — I favor beginning my assessment with a Systematic Approach. Descriptive analysis of the ECG in today's case reveals a regular, narrow tachycardia at ~130/minute, without clear sign of sinus P waves.
- QRS amplitude appears increased in several chest leads (ie, very deep S waves in leads V1,V2 — large isoelectric complex in V3).
- There appears to be a Q wave in lead aVL — though limb lead artifact makes this difficult to assess.
- As per Dr. Smith — T waves in multiple leads are tall, peaked, and manifest a narrow base. This is especially true in leads V2,V3 — in which T wave amplitude exceeds 15 mm! Of note — these T waves are symmetric, with similarly angled ascending and descending limbs of the T wave.
- BOTTOM LINE: As per Dr. Smith — this ECG is diagnostic of Hyperkalemia until you prove otherwise.
- What is the rhythm?
- Given how tall the T waves are and the lack of P waves — Why isn't the QRS wide?
- Why isn't the serum K+ higher than 6.2 mEq/L?
- Why is there T wave inversion in leads I and aVL?
- Finally — Could anything else be going on with this patient?
Dr. Smith suggests that the rhythm in today's case is sinoventricular rhythm — because it is common with hyperkalemia for sinus node activity to continue (at least for a while) despite the disappearance of P waves on ECG.
- In today's case — I fully acknowledge that I do not know for certain what the rhythm is. The QRS is narrow — and no P waves are seen. But the rate is ~130/minute — which is a bit fast for sinus tachycardia. So IF this is sinus tachycardia with a sinoventricular rhythm — then we have to explain WHY the rate is this fast.
- Alternatively — the rhythm could be junctional tachycardia ...
- Finally — it almost looks like there are 2 equally spaced upright deflections in lead aVR, which if true might indicate 2:1 AFlutter.
- BOTTOM Line: Practically speaking — it does not matter what the rhythm in today's case is — because IF this patient would be promptly treated with Calcium — whatever this rhythm was would most probably rapidly resolve.
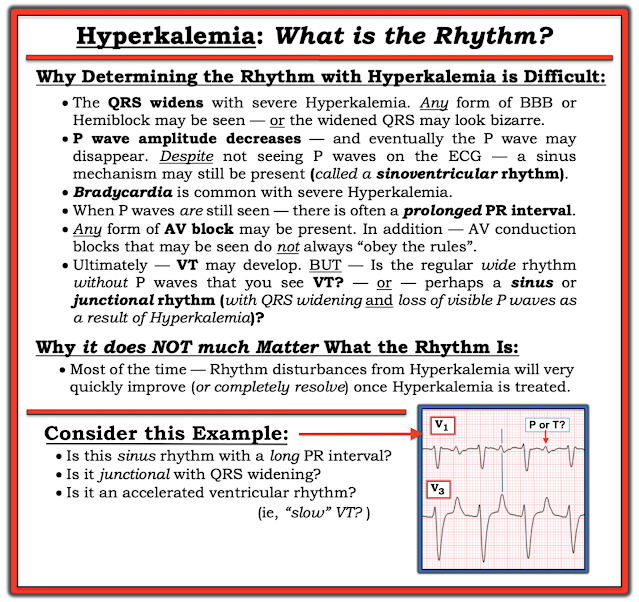 |
| Figure-1: Reasons for the difficulty determining the rhythm with severe hyperkalemia. |
- TO EMPHASIZE — Not all patients follow the sequence of ECG changes shown below in Figure-2. For example — some patients may develop everything except QRS widening. Others may not show T wave peaking — or may only show this finding as a later change. And despite marked hyperkalemia — some patients may not show any ECG changes at all.
- The above said — Over the years, I have found Figure-2 to be helpful as a guide that does hold true in a significant percentage of patients.
- P.S.: There are times when even before the serum K+ value returns from the lab — you know from the ECG that there is severe (life-threatening) hyperkalemia. For example — marked bradycardia with unusual forms of advanced AV block — or marked bradycardia without evident P waves — or marked QRS widening with "shapeless" morphology — are all ECG indication of the need for immediate IV calcium until improvement of these ECG patterns.
 |
| Figure-2: The “textbook” sequence of ECG findings with hyperkalemia. (I've reproduced this figure from My Comment in the January 6, 2020 post of Dr. Smith's ECG Blog). |
- As emphasized above — the "textbook" sequence shown above in Figure-2 is not perfectly followed by all patients.
- Certain conditions (ie, DKA) may be associated with rapid intra-extracellular K+ shifts — such that serum values can change quickly.
- There is often missing documentation as to when which ECG was recorded at the time of which blood draw (and whether any treatment had yet been initiated). So the 6.2 mEq/L K+ value may (or may not) closely correlate to the timing of today's ECG.
- Aren't those deep, symmetric T wave inversions in leads I and aVL the virtual "mirror-image opposite" of the tall, pointed upright T waves in leads III and aVF?
- The ECG of a patient with hyperkalemia shows the net effect of what underlying ST-T waves looked like before development of the tall, peaked T waves of hyperkalemia. Only after correcting hyperkalemia and repeating the ECG — will you be able to determine whether ischemic ST-T wave changes exist.
- This point is especially relevant in today's case — because the T waves in many leads are especially tall (and there is also deep T wave inversion in leads I and aVL). TO EMPHASIZE — Although I suspect that all ST-T wave abnormalities will normalize with correction of the hyperkalemia in today's case — we do not know this for certain without repeating the ECG.
- The other reason why the ECG in today's case should have been repeated after correction of hyperkalemia — is that the only cardiac rhythm documented in this case is an SVT at ~130/minute without sinus P waves. We do not know for certain what the rhythm was? And, there is no documentation that the tachycardia has resolved.




-USE.png)

-USE.png)





-USE.png)