This was contributed by Hans Helseth (he will start medical school soon). With edits and additions by Smith and Grauer.
A 75 year old man with hypertension and hyperlipidemia presented to the emergency department by EMS for 1.5 hours of chest pain with vomiting. Paramedics administered 3 doses of sublingual nitro and 4 baby aspirin, neither of which relieved the pain.
His vital signs were normal.
His ED EKG was recorded at 09:04 with ongoing chest pain:
There is sinus rhythm at 61 BPM. The QRS and T duration, axes, and morphology are normal.
So, YES, this is a completely normal EKG.
An old EKG from three years ago was available for reference:
It is the same.
Dr. Balasubramanian wrote to say he does not think the ECG is normal:
"Dear Dr Smith, The ED - ECG clearly shows
straightened ST in aVL, clearly appreciated on comparison with the ST
segment of flanking leads II & V2 ( as commented by Dr Ken
Grauer also).. Also this is a new development compared to old ECG. Next, please note N-WAVES in II, III, aVF, V5 & V6. These waves occur in LCX OMI. These N-Waves are well seen in the second ECG. They are not visible in the old ECG.
(N-waves are also called "delayed activation waves")
Smith: I don't see N-waves, and whatever straightening there is in aVL, I don't see.
I do not discount the possibility that there are things that I just cannot see. I frequently see things which other self proclaimed experts cannot see. Just because you can't see something on an ECG does not mean it is not there.
The Queen of Hearts sees zero evidence of OMI, though that does not mean that she thinks it is completely normal. I still think it is completely normal, even after taking Dr. Balasubramanian's comments into account. If I think it is normal and the Queen of Hearts sees nothing, can I teach anyone out there to see the findings of Dr. B and believe that they are specific? No.
There is no way you would suspect OMI from this ECG alone. You might activate the cath lab based on the clinical presentation alone, as it is VERY high risk.
_________
The ED provider correctly interpreted this EKG as normal. The patient had normal vital signs and blood work except for a HS troponin T which, at 09:14, was measured at 32 ng/L (Reference range 6-15).
_______
Smith: This is simple. This patient has chest pain and an otherwise unexplained elevated troponin (an elevated troponin from chronic myocardial injury could be explained if the patient had heart failure or renal failure on dialysis). (Acute myocardial injury NOT due to acute MI could be explained by conditions such as pulmonary embolism, takotsubo, myocarditis, and more). There is nothing to suggest any diagnosis compatible with acute or chronic myocardial injury.
Thus, this is acute myocardial infarction by definition of the 4th Universal definition of MI, regardless of the ECG. Is it type 1 MI or type 2 MI? (Type 1 is due to ACS; Type 2 is due to supply/demand mismatch). There is nothing to suggest supply/demand mismatch of type 2 MI. Supply: anemia, hypotension, hypoxia. Demand: severe tachycardia, severe hypertension.
Any acute type 1 myocardial infarction that has persistent chest pain unresponsive to aspirin and nitroglycerin needs to go emergently to the cath lab. This is according to ALL NSTEMI guidelines of the ACC/AHA and also ESC.
Thus, the patient should receive sublingual, or IV bolus, nitroglycerin to the point his blood pressure will not tolerate it or until the pain resolves. If the pain does not resolve, the cath lab should be activated.
This is how it should work (2 previous posts):
_________
At 11:02, the troponin rose to 48 ng/L. An EKG was repeated at 12:53 due to ongoing chest pain and rising troponin:
The heart rate has dropped slightly. It is otherwise unchanged.
At 13:11, the troponin again rose, this time to 80 ng/L. The ED provider discussed the case with cardiology, who recommended holding heparin and taking the patient for a CT coronary angiogram. The recommendation was to discharge the patient if the scan was normal. At 14:22, the scan resulted. Here is a screenshot from the scan:
There is a darker area across the basal lateral wall representative of transmural ischemia. The scan was interpreted as showing:
- A potentially flow-limiting LAD lesion
- Total Cx Occlusion with ongoing Acute MI
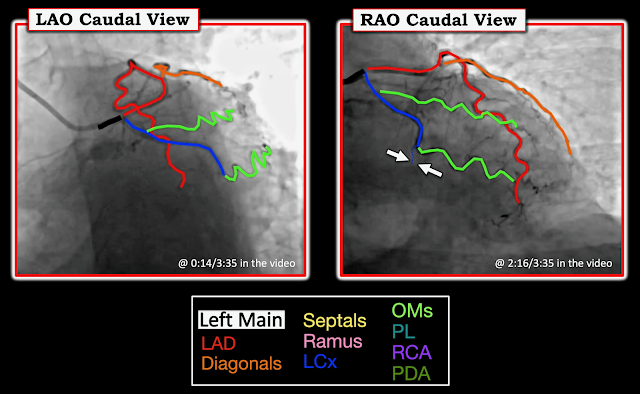
Cardiology accepted the patient for catheterization. The cath lab was prepped and the patient was taken for invasive coronary angiography at 16:04. Willy Frick has kindly annotated and narrated the cath shots:
Ken Grauer also created this figure for reference:
There is a plaque rupture with subtle total thrombotic mid Left Cx occlusion. The thrombus was aspirated and the lesion stented.
No EKGs or troponins were recorded after angiography. An echo the next day showed basal to mid lateral hypokinesis with an estimated EF of 55-60%. The patient was discharged two days later with a diagnosis of NSTEMI.
_______________________________________
It is possible for the EKG to be completely normal despite ongoing Occlusive Myocardial Infarction (OMI). Cases like these emphasize the importance of serial troponin testing and emergent catheterization for refractory chest pain. This case also demonstrates a great flaw in "NSTEMI". The pathology here is identical to that which has been called "STEMI" -acute plaque rupture with total thrombotic coronary artery occlusion. Why should the diagnosis be different just because it is not apparent on the EKG? The diagnosis is apparent by every other measure: Symptoms, troponin, CT, invasive angiography, echocardiography.
The AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes recommends immediate (within 2 hours) invasive angiography for patients with refractory angina (see page 30). However, Lupu et al. found that these guidelines are followed only 6.4% of the time.
Learning points:
- The EKG can be completely normal in acute OMI
- Angiography within two hours is recommended for patients with refractory chest pain and evidence that the chest pain is due to acute coronary syndrome (and is thus "angina")
- One elevated troponin in a patient with new chest pain and no other reason for troponin elevation is acute MI.
- If that chest pain is refractory, it is OMI until proven otherwise and needs emergent cath lab activation.
- The paradigm of acute MI should be based on the underlying pathology (occlusion), not on any ECG feature. We should abandon "STEMI/Non-STEMI" in favor of "OMI/NOMI". OMI/NOMI recognizes that
- 1) there are ECG features beyond ST Elevation for diagnosing OMI and
- 2) sometimes the ECG does not show OMI even though OMI is present, and we need to use other modalities, up to and including angiography, to find it.
===================================
MY Comment, by KEN GRAUER, MD (5/4/2025):
===================================
I found today's case by Hans Helseth both interesting and insightful for a number of reasons:
- This patient's initial ECG is normal (or at least — it looks almost normal ... ).
- The 2nd (and last) ECG done in this case — is not significantly different from the initial tracing (ie, also interpreted as a "normal" ECG) — yet cardiac catheterization showed acute LCx occlusion.
- The acute LCx on cath is subtle, and potentially easy to overlook. But as demonstrated in the above superb narrative description by Dr. Frick — there is no doubt about the LCx occlusion. The "lesson" is that dependence on the 2 non-diagnostic ECGs and the modest Troponin elevation seen in today's case could have easily resulted in premature discharge of this patient.
- Cardiac cath was eventually performed at 16:04 — which was 7 hours after the initial ECG. This is about 5-to-6 hours later than when cath should have been done. And while I never like being critical in the "retrospectoscope" (especially regarding cases in which I was not there — and for which I lack important information) — there are a number of important oversights in this case that merit attention, so that management of similar cases can be improved.
Was the Initial ECG "Normal"?
I have previously addressed the issue of how we define an ECG as "normal" (See My Comment in the January 15, 2024 post and the March 12, 2025 post in Dr. Smith's ECG Blog).
- "My Take" on this Question (from the Jan. 15, 2024 post): The definition of a "normal" ECG — is dependent on the clinical circmstances under which the tracing is recorded and dependent on the person who is interpreting the tracing.
- Both the clinical circumstances and the person who is interpreting the tracing are critically important.
For example — In Figure-1 I have reproduced today's initial ECG and the prior ECG done 3 years earlier. Imagine 2 clinical scenarios.
Clinical Scenario #1:
- What if ECG #1 was obtained from a previously healthy young adult admitted through the ED for abdominal pain — but no CP.
- My Interpretation — Given this clinical scenario, I would interpret ECG #1 as showing some minimal nonspecific ST-T wave changes that do not look acute. I would not order Troponins in this patient — and repeat ECGs would not be indicated.
-USE.png) |
| Figure-1: Comparison between today's initial ECG — with a prior ECG from 3 years earlier. |
Clinical Scenario #2:
- What if this same ECG #1 was instead obtained from a 75-year old man who was brought to the ED by EMS with a 1.5 hour history of chest pain and vomiting — with this CP not relieved by NTG — and with ongoing CP still at the time ECG #1 is recorded.
- My Interpretation — Given this clinical scenario (which is precisely the clinical scenario for the patient in today's case) — even before I look at this ECG, I know I am confronted with a higher-risk patient for having an acute event.
- As a result — my threshold for interpreting ECG #1 as potentially suspicious for an acute event will be dramatically lowered.
- To Emphasize: I am definitely not saying ECG #1 is diagnostic of an acute event. On the contrary — ECG #1 is a non-diagnostic ECG. But — given the clinical scenario of today's case (and before I looked at what happened in today's case) — I thought the T waves in both high-lateral leads looked slightly more "bulky" than expected (RED arrows in Figure-1) — and I thought there was the suggestion of subtle ST segment straightening in lead II. I did not see other changes — but given the history of Clinical Scenario #2 — I wondered if this might be LCx OMI?
What (if anything) To Do Next?
- As I mentioned above, in the case of Clinical Scenario #1 — Given the absence of CP in this previously healthy young adult admitted for abdominal pain — I would not order Troponins, and I would not repeat the ECG.
- In contrast, for Clinical Scenario #2 (which is the scenario of today's patient) — given the history of new-onset severe CP not relieved by NTG X 3 — We need to get serial ECGs and serial Troponins. And especially given ongoing severe CP that this patient was experiencing — the 1st repeat ECG should be obtained within 10-20 minutes (ie, not later than 9:24).
- Instead — the ECG was not repeated until 12:53 (which is nearly 4 hours after the initial tracing was done! ).
- Even after the initial Troponin came back elevated (32 ng/L — with a normal range = 6-15 ng/L) — and even after a 2nd Troponin came back more elevated (to 48 ng/L at 11:02) — the ECG was not repeated until 12:53.
NOTE: The repeat ECG was correctly interpreted as not showing significant change compared to the 1st tracing. That said:
- As per Hans Helseth's above discussion — persistent ischemic-sounding CP (especially for severe CP lasting >1-2 hours), even in the absence of diagnostic ECG changes — is indication for cardiac cath to define the anatomy (ie, To rule out an acute cardiac event).
- This indication for cath when ischemic-sounding CP persists is much stronger in today's case because of the abnormal (and increasing) Troponin values.
- KEY Point: Just because neither of the 2 ECGs that were done were diagnostic of an acute cardiac event in no way rules out the possibility that diagnostic ECG changes might have occurred, but simply were not captured because providers waited nearly 4 hours to repeat the initial tracing.
==============================
Consider Clinical Scenarios #3 and #4 ...
==============================
Clinical Scenario #3:
- What if CP continued at the same intensity from 9:04 (when the initial ECG was done) — until 12:53 (when the repeat ECG was done).
- My Interpretation — Given no change in symptoms during the nearly 4 hours that passed between the recording of ECG #1 and ECG #2 — we can say that despite ongoing CP, the ECG failed to show evidence of an acute event. Sometimes this happens. Even so — the rising Troponin in association with persistent ischemic-sounding CP was indication for cardiac cath several hours before that repeat ECG eventually got done.
Clinical Scenario #4:
- What if instead — this patient's CP totally resolved 30-to-60 minutes after ECG #1 was obtained — only to return 10 minutes later, much more severe than at any time up until then. But 15 minutes after that — while still present, the patient's CP returned to the same (less-than-maximal) intensity level that he reported at the time the initial ECG was done.
- My Interpretation — A "golden opportunity" would have been lost if no ECG was done at the time this patient's CP resolved — and, if no ECG was done 10 minutes after that when the patient's CP was maximal.
- KEY Point: It is very possible with Clinical Scenario #4 — that a dramatically different ECG picture might have been obtained when the patient's CP resolved — and, it is even possible that STEMI criteria might have been satisfied IF a repeat ECG had been obtained 10 minutes after that when his CP became maximal.
==============================
Additional Learning Points:
- Whether an ECG should be called "normal" — depends on both the clinical circumstances under which the tracing is recorded — and — dependent on the person who is interpreting the tracing.
- The 7 hours it took for cardiac cath to be performed in today's case might have been substantially reduced if the following important principles were followed: i) A repeat ECG should be routinely obtained within ~20-30 minutes of the initial tracing when a patient presents to the ED for new ischemic-sounding CP; ii) Additional ECGs should be obtained whenever the patient's symptoms change until a definitive diagnosis of OMI or non-OMI can be made; and, iii) The presence and relative severity of CP (ie, on a scale of 1-to-10) should be noted in the chart at the time that each ECG is recorded.





No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.