Written by Pendell Meyers
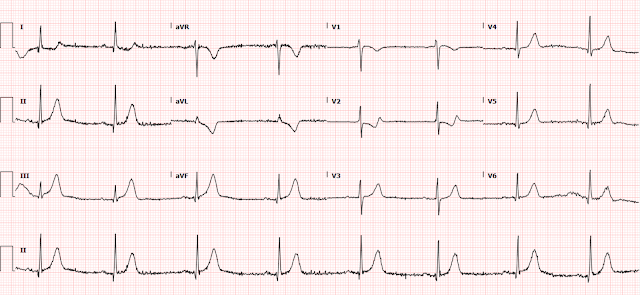
An elderly man with history of CAD presented to the ED with acute chest tightness and diaphoresis beginning 30 minutes prior to arrival. He was noted to be bradycardic and hypertensive on arrival.
 |
| What do you think? |
 |
| Interval improvement in inferior leads, and posterior reperfusion T waves, all signaling successful reperfusion. |
 |
| Further ECG evolution of reperfusion. |
Next AM echo:
EF 59%, hypokinesis of the basal inferior myocardium.
2 weeks later:
Still further evolution
See how this case beautifully demonstrates the OMI and reperfusion ECG sequences:
He was discharged in good condition.
Learning Points:
This patient got optimal care only by violating the current STEMI guidelines and diagnosing OMI despite lack of STEMI criteria.
You must be able to see hyperacute T waves to diagnose OMI accurately.
Reciprocally inverted hyperacute T-waves in aVL are a reliable sign of inferior OMI.
ECGs during OMI and reperfusion usually follow the OMI paradigm ECG sequences. Learning this progression allows you to understand the state of the artery, diagnose OMI sooner than STEMI criteria, etc.
- I focus my comments on a number of different aspects relevant to the interpretation of the first 3 ECGs shown by Dr. Meyers in today's case.
- With this presenting history — we essentially need to be looking at the initial ECG thinking this patient is likely to be having an acute cardiac event until we can prove otherwise.
- As per the sequential Figure shown above by Dr. Meyers that illustrates the ECG evolution of acute coronary occlusion and reperfusion — the hyperacute T wave stage typically occurs before the stage of ST elevation.
- Even before seeing the baseline tracing ( = ECG #2 in Figure-1) — it should be obvious that T waves in the inferior and lateral chest leads are disproportionately peaked and "hypervoluminous" (especially in leads III and aVF) with respect to R wave dimensions of the QRS complex in respective leads. The reciprocally-inverted hyperacute T wave in lead aVL confirms the diagnosis of acute inferior OMI. Waiting until ST segments elevate would only delay the inevitable at the cost of valuable myocardium.
- As I've alluded to in multiple posts in Dr. Smith's ECG Blog — I favor the Mirror Test as a visual aid for facilitating recognition of the acute ST-T wave changes of acute posterior MI as they are seen in the anterior leads (See My Comment in the January 3, 2022 post). Typically — a shelf-like shape of ST-T wave depression is initially seen in one or more anterior leads, with no more than modest terminal T wave positivity.
- Instead, in ECG #1 — there is virtually no ST depression in leads V2 and V3. I thought the T wave in lead V3 was disproportionately positive — and the terminal T wave positivity in lead V2 was more than expected.
- My Impression of ECG #1: I completely agree with Dr. Meyers that the acute inferior OMI in the initial ECG in today's case was obvious. But I thought the ST-T wave appearance of leads V2, V3 in ECG #1 already suggested posterior reperfusion T waves (in which anterior ST depression resolves — and anterior T waves become taller and more peaked).
- I thought the mirror-image view of leads V2,V3 in ECG #1 supported my impression (RED inserts of inverted leads V2,V3 showing beginning T wave inversion in V2 — and deep, symmetric T wave inversion in lead V3).
- In further support that this ST-T wave appearance in leads V2,V3 of ECG #1 represented early reperfusion changes before this was seen in other areas of the heart — is the change compared to the baseline ECG from 2 years earlier — and — the further progression of anterior T wave peaking seen in ECG #3, that was done 3 hours after ECG #1 (See the comparison between ECG #1 and ECG #3 in Figure-2 below).
- We can only speculate on the reason as to why the posterior wall might show reperfusion T waves at the same time that inferior and lateral chest leads show the hyperacute T waves of acute occlusion. Perhaps this is related to the 2 distinct RCA lesions? (noted proximally and mid-vessel on cath) — or perhaps due to multi-vessel disease? (which was also noted on cath).
- WHY in ECG #2 is QRS morphology changing for beats #1 and 2 in lead III — and for beats #3,4,5 in lead aVF?
-USE.png) |
| Figure-1: Comparison of the initial ECG in today's case — with a baseline tracing done 2 years earlier. RED inserts in ECG #1 show the Mirror Test applied to leads V2 and V3. |
- This is a phenomenon that I have occasionally observed over the years, that in my experience is unique to these 2 leads. I believe the reason for this phenomenon — is that the heart sits on the diaphragm, and these 2 inferior leads (leads III and aVF) view the heart's electrical activity from a perspective directly below this. As a result — these leads are sometimes subject to beat-to-beat variation in QRST morphology as a result of diaphragmatic motion associated with accentuated breathing. I have not observed this phenomenon in other leads.
- Awareness of this phenomenon is important — because of the potentially confounding effect it may have on assessing acute changes in the inferior leads. On occasion — a longer lead sample of leads III and aVF may be needed to determine the "true" QRST morphology in these 2 leads.
- What is the rhythm in ECG #3?
-USE.png) |
| Figure-2: Comparison of the initial ECG in today's case — with ECG #3 (done post-Cath — which was ~3 hours after ECG #1). |
- Clearly there is a marked sinus bradycardia in the long lead II rhythm strip of ECG #3. But isn't there also alternating longer-then-shorter R-R intervals? The duration of each of these longer R-R intervals (ie, between beats #1-2; 3-4; and 5-6) is virtually equal — and — duration of each of these shorter R-R intervals (ie, between beats #2-3; 4-5; and 6-7) is also virtually equal. Isn't this more than what you would expect by chance? This is not the typical phasic variation of R-R intervals over a longer series of beats that is expected with sinus arrhythmia.
- I strongly suspect that the rhythm in Figure-2 represents 3:2 SA block. The clinical setting for this uncommon form of conduction disturbance is present in today's case (ie, an elderly man, therefore more susceptible to Sick Sinus Syndrome — who presents with acute inferior infarction).
- SA Block is not common. I count on my fingers and toes the number of times I've seen true SA block over my decades of looking for this rhythm disorder. But as per my proposed laddergram in Figure-3 — I believe this a possible (if not probable) diagnosis for the bradycardia and group beating that we see in the long lead II of ECG #2.
- I've excerpted the essentials of SA block from my ACLS-2013-ePub in Figure-4.
-USE.png) |
| Figure-3: My proposed laddergram for the rhythm in ECG #3. |
-USE.png) |
| Figure-4: Essentials of SA Block (Modified from Grauer: ACLS-2013-ePub). |





No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.