A 30-something male presented in the middle of the night with several hours of sharp, non-radiating, left sided chest pain. It was there earlier, went away, and then returned approximately 1 hour prior to arrival. He is a smoker and has some family history of early MI.
Exam and vital signs were normal.
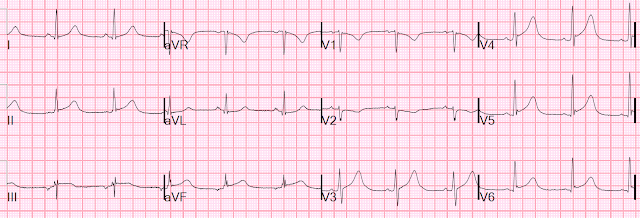
Here was the triage ECG:
Providers were not convinced that this was OMI, so they awaited the first troponin. The initial high sensitivity troponin I returned 68 minutes after this ECG at 3900 ng/L (quite high, consistent with OMI, NOMI, or other etiology of acute myocardial injury).
Given the young age, they were also suspicious of myocarditis, and ordered a CRP.
The Cath lab was activated. Here is the report:
Cath lab activation at 3 am by the ED for atypical CP, and elevated troponin with diffuse STT changes. No angiographically significant obstructive coronary artery disease .
Peak trop at 7 hours was 4646 ng/L
CRP 88 (very high)
Formal Echo the next day:
The estimated left ventricular ejection fraction is 49%.
Cardiac MRI
1) Borderline decreased LV function with small wall motion abnormality involving the apex
2) Normal dimensions of all cardiac chambers
3) Patchy areas of myocardial edema. There is also patchy myocardial delayed enhancement with subendocardial sparing, involving the distal anterior wall, distal inferolateral wall and the basal inferior wall.
Pattern is consistent with acute myocarditis.
4) Trace pericardial effusion.
After the fact, this further history was obtained:
Of note, one week ago he was ill with nausea, vomiting, and diarrhea. He has noticed fevers and chills as well.
Subsequent ECGs?? I would love to have seen the evolution of the ECGs over days to weeks, but unfortunately, no more were recorded.
Learning points:
Sometimes there are false positive ECGs, or at least a clinical scenario and ECG combination that forces an angiogram. How could such a false positive activation be avoided?
That is very difficult, because the delays inherent in confirming or rebutting the diagnosis of OMI take a lot of time, and time is myocardium.
Cases like this are NOT common, and so will not lead to a flood of unnecessary angiograms.
If suspicion of Non-OMI etiology is high, then emergent formal bubble contrast echo is very useful, but in myocarditis, it usually reveals a wall motion abnormality.
CT coronary angiogram is excellent, but is rarely available outside of business hours, and hardly ever at night.
The initial troponin is often negative in OMI, and even if it were useful, the mean time from presentation to sample collection in MI studies is about 50 minutes, and the time from collection to central laboratory result is at least 30 minutes. Although the POC troponins that are available at the present time are very inaccurate in the low range and not appropriate for rule out, they can be useful in confirming acute MI (OMI or NOMI) if elevated.
But they do NOT differentiate between OMI and myocarditis!!
Bottom line: if you don't want to miss OMI, with its attendant significant myocardial loss, then some false positive angiograms are a reasonable price to pay.
See this case:
A Young Woman with Chest Pressure and Subtle, Focal ST Elevation and Depression
MY Comment by KEN GRAUER, MD (5/24/2022):
===================================
- By far — the most common lead reversal is mix-up of the LA (Left Arm) and RA (Right Arm) electrodes. But this is not the mix-up that occurred in today’s case — because we do not see global negativity (of P wave, QRS and T wave) in lead I (See the February 11, 2020 post).
- In the July 28, 2020 post in Dr. Smith’s ECG Blog — I cited my favorite on-line “Quick GO-TO” reference for the most common types of lead misplacement, which comes from LITFL ( = Life-In-The-Fast-Lane). Simply put in, “LITFL Lead Reversal” into the Search bar — and the link comes up instantly!
- The “tipoff” to LA-LL Reversal in Figure-1 — is that the P wave in lead I is clearly larger than the P wave in lead II (and that is distinctly unusual when there is sinus rhythm).
- The other, more subtle "tipoff" to LA-LL Reversal — is that in the context of what appears to be hyperacute ST-T waves with predominantly positive QRS complexes in leads I and II — the predominantly negative QRS, which also manifests some ST elevation in lead III just looked "off".
- Take-Home Message: Remember that with normal sinus rhythm — it is rare indeed that the P wave in lead I will be larger than the P wave in lead II. Next time you see this — Enter "LITFL Lead Reversal" into your internet search bar to remind yourself of what you'll see with the common types of lead reversal.
- P.S.: For another example of LA-LL Lead Reversal like the one in today's case — Go to the Addendum at the bottom of the page in the August 28, 2020 post in Dr. Smith's ECG Blog. I initially missed that one ...

-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.