Written by Pendell Meyers
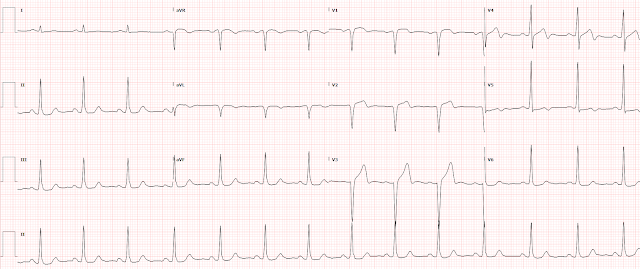
Before we get to the whole case, let's interpret this ECG without any other context except to say that this is a 49 year old man with acute onset chest pain:
Here is the whole case:
A 49 year old man with no medical history presented with acute onset chest discomfort for several hours which improved to 2/10 severity at the time of arrival to the emergency department.
Here is his triage ECG (ECG1) at 1750:
 |
| What do you think? Form your opinion, then see the baseline ECG below and see if your opinion changes. |
 |
| Clear STEMI criteria are now met, also with enlarging hyperacute T waves in V1-V4. Reciprocal STD in II, III, aVF, and V6. |
 |
| Continued reperfusion. |
Learning Points:
When reperfusion T wave inversions suddenly go away and are replaced by upright T waves, in the presence of ischemic symptoms, this is diagnostic of reocclusion as seen above (this is known as pseudonormalization).
Understanding the OMI progression of occlusion and reperfusion gives you a much better understanding of ACS and OMI than the STEMI paradigm, and allows you to detect OMI sooner which improves the efficacy of reperfusion therapies.
NOTE: The numbering of my Figures in this case is OFF — because Drs. Smith and Meyers published this case on December 4, and they changed the sequence in which they show the tracings after I had already written my comment (which I had done on November 23, 2020). As a result, please consider My Comment independently. I believe there are still lessons to be learned by reading My Comment as a separate and supplementary discussion. THANK YOU — Ken Grauer, MD (12/6/2020).
===================================
MY Comment by KEN GRAUER, MD (11/23/2020):
===================================
One of the main “Take-Home” points from today’s case is the following: This is why serial tracings are done.
- Imagine the only ECG you are shown is the one that you see in Figure-1. This is the 3rd ECG that was shown in the discussion by Dr. Meyers above — done just 16 minutes after the 1st ECG that was shown above.
- You are told the patient is a previously healthy 49-year old man who presented with chest pain over the previous few hours. His symptoms had improved — but chest discomfort was returning at the time the ECG in Figure-1 was obtained.
Given this history — IF the ECG in Figure-1 was the only tracing you were shown — HOW would you interpret this ECG?
Figure-1: The 3rd ECG that was shown above in today’s case. Imagine this was the only ECG that you saw. HOW would you interpret it? (See text).
HOW Would You Interpret the ECG in Figure-1?
The rhythm in ECG #3 is sinus at ~90/minute. The PR – QRS – and QTc intervals are all normal. The frontal plane axis is normal at about +75 degrees. Voltage criteria for LVH are not satisfied.
Regarding Q-R-S-T Changes:
- There is a QS complex in lead aVL — and QS complexes in leads V1 and V2.
- Regarding R wave progression — after the QS complexes in leads V1 and V2, a tiny-but-present r wave isseen in lead V3. So, R wave progression in the anterior leads is poor — even though transition occurs normally between leads V3-to-V4.
- Regarding ST-T wave changes — there are a number of nonspecific findings. In the limb leads, the ST-T wave in lead I is flat — there is nonspecific ST segment flattening in the inferior leads — and there is shallow T wave inversion in lead aVL.
- In the chest leads — anterior lead ST-T wave appearance is not necessarily abnormal. There appears to be slight J-point ST depression in leads V4-thru-V6.
IMPRESSION: If ECG #3 was the only tracing you saw — the findings would be nonspecific.
- The shallow T wave inversion in lead aVL is not necessarily abnormal as an isolated limb lead finding — given the relatively vertical frontal plane axis and negativity of the QRS complex in lead aVL.
- Although the QS complexes in leads V1 and V2, in association with no more than a tiny r wave in lead V3 could reflect anteroseptal infarction at some point in time — these findings could also be the result of faulty lead placement or LVH (even though voltage criteria for LVH are not satisfied) or chest wall deformity.
- The lateral chest lead J-point ST depression could be ischemic. That said — this is a nonspecific finding that may or may not be acute.
- BOTTOM Line for ECG #3: If this was the only ECG you were shown — there would be NO way to know if an acute event was ongoing.
COMMENT: As per Dr. Meyers, the reason there is NO way to know from ECG #3 alone that there is an ongoing acute event — is that this ECG represents “pseudonormalization”. It’s easiest to appreciate this phenomenon by putting the first 3 tracings shown above in this case together (Figure-2).
- TAKE another LOOK at these first 3 tracings that were shown above. Given that this patient’s chest pain that prompted his ED visit had almost resolved by the time ECG #1 was obtained — Was it necessary to find the baseline tracing ( = ECG #2) in order to make the diagnosis?
- WHAT ELSE do you see in these serial tracings?
MY Thoughts regarding Figure-2:
Given the history of several hours of new chest pain that had almost resolved at the time the initial ED ECG was recorded — this ECG #1 is consistent with Wellens’ Syndrome.
- The picture of the ST-T wave in lead V4 is typical of Wellens. As per Dr. Meyers — the steep downsloping from the peak of the T wave in V4, that finishes with a biphasic terminal negative component is diagnostic of reperfusion given the clinical setting.
- Looking closely — terminal T wave negativity is suggested in neighboring leads V3 and V5.
- Typically with Wellens’ Syndrome — frank infarction should not yet have occurred. Given this patient’s waxing and waning symptoms and QS complexes in leads V1-thru-V3 — this is difficult to ascertain. But what can be said — is that there is NO way that the ST-T wave appearance in lead V4 is “normal”.
- In support of an evolving LAD occlusion is the hyperacute ST-T wave in lead V3. For clarity (given overlap with the R wave in the long lead II rhythm strip below it) — I’ve drawn in RED the depth of the S wave in lead V3 — and in BLUE the ST-T wave in this lead. Given relatively modest S wave depth — I interpreted the ST-T wave in lead V3 as more “voluminous” than-it-should-be, therefore hyperacute given the clinical setting.
- Assessment of the ST-T waves in leads V1 and V2 is more subtle. In isolation — I would have been uncertain about these leads. But in the context of clearly abnormal ST-T waves in leads V3 and V4 — the slight-but-real ST coved elevation in lead V1 and the slight ST elevation with clear ST segment straightening in lead V2 seem likely to be a part of the same process.
- Finally — there appears to be slight-but-real ST depression in lead V6.
- BOTTOM Line: Given the history in this case — I thought ongoing LAD occlusion was strongly suggested from ECG #1, even before looking at the baseline tracing.
As per Dr. Meyers — finding the baseline tracing on this patient ( = ECG #2) confirmed my above suspicions about ECG #1.
- The QS with shallow T wave inversion in lead aVL was previously present — so that was not a new finding in ECG #1.
- Otherwise, comparison of ECG #2 with ECG #1 reveals that there has been loss of R wave amplitude in lead V3 (which has become an QS complex in ECG #1) — and all of the above-described ST-T wave changes in ECG #1 are new compared to the baseline tracing.
I’ll conclude by comparing ECG #3 with the initial ECG done in the ED just 16 minutes earlier. The reason ECG #3 was done — was return of this patient’s chest pain. As per Dr. Meyers — there is pseudonormalization in ECG #3, caused by reocclusion of the LAD, that results in loss of the reperfusion T wave inversion seen in ECG #1.
- As per the initial point I emphasized — Today’s case illustrates why serial tracings are done. IF a definitive diagnosis of ongoing LAD occlusion had not already been made from ECG #1 — it should have been made by interpretation of the 3 tracings shown in Figure-2, given the context of minimal symptoms with ECG #1, and return of severe chest pain with ECG #3.
- The need for prompt cath + PCI could have been established before the frank ST elevation seen in the 4th ECG.








Thank you very much for your blog!
ReplyDeleteTheese cases are just astounding!
Please never stop posting.
You are well known all around the world.
Greetins from Argentina.
Thank you Rafa from Argentina!!
Delete