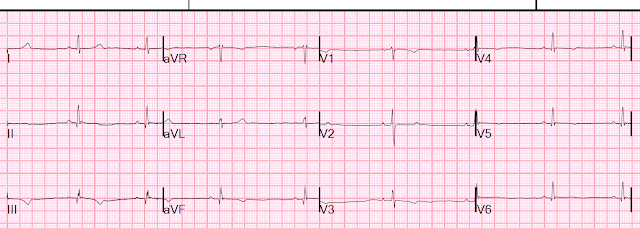
I (Smith) was asked to look at this ECG (ECG-4).
What do you think?
I said there is an inferior and lateral myocardial infarction, with Q-waves, and it is recent.
They added some history: the patient had a STEMI 1 week ago.
They then showed me the most recent previous ECG (ECG-3), recorded 1 day after intervention for that inferior STEMI. They were worried that the T-waves were much deeper in ECG-4 than in ECG-3, and that this was therefore evidence of recurrent MI.
ECG-3
The T-waves are inverted in II, III, and aVF, as well as V4-V6.
They are less deep than in ECG-1
Notice also that the T-wave in V2 is larger on ECG-4 than ECG-3.
So there is deepening T-wave inversion -- is it due to new ischemia??
Here are all the ECGs so you can see them in order (the first is ECG-1 from a week prior):
Initial troponin = 4 ng/L Upper reference for women is 16 ng/L.
So, like many STEMI, the initial troponin is negative.
Deepening of the T-wave is the normal progression after reperfusion of STEMI. These are analogous to Wellens' waves, but of the inferior wall and due to PCI, not spontaneous.
The deepening inversion is NOT an indication of new ischemia.
Here are the 3 post PCI ECGs in this case. Notice the progressive T-wave inversion.
After PCI (ECG-2)
Slightly deeper T-wave inversion -- normal evolution
7 days after PCI (ECG-4, again)
She had serial troponins measured (Abbott high sensitivity TnI). Unfortunately, they had not been measured to peak during her STEMI admission. One can guess that they might have peaked at 10,000 - 40,000 ng/L.
Trop 1 = 1006 ng/L
Trop 2 = 957 ng/L
Trop 3 = 952 ng/L
These are very high but falling, consistent with her infarction 7 days prior.
She was discharged from the ED.
What would these T-waves do if there was re-occlusion? They would flip upright! They might even look normal! (They would NOT get deeper -- deepening is a good sign!). That is why "normalization" (becoming upright) of such T-waves is called "Pseudonormalization". In other words, what looks normal is not and is actually dangerous.
After weeks to months the T-waves will normalize. So it is only pseudonormalization if it is early after the infarct (perhaps up to weeks?)
There are many cases of pseudonormalization on this blog. Here are a few of the many:
Subtle LAD Occlusion with Pseudonormalization of Wellens' Waves.
Pseudonormalization of Wellens' Waves
Pseudonormalization of Inferior T-waves
Learning Points
1. Reperfusion results in inversion of T-waves and progressive deepening as evolution progresses over time. Initially there is terminal T-wave inversion, then it deepens over hours to days. Re-occlusion at any time will result in pseudonormalization.
See the below schematic from my book. The ECG in Acute MI.
Upper left is normal. From that position, the artery can reperfuse (and the ECG evolution goes to the right from there), or it can remain occluded (going down). At any point in time during the persistent occlusion, it may spontaneously (or through therapy) reperfuse, in which case it will evolve to the right. Re-occlusion is not shown in this graphic.
===================================
MY Comment by KEN GRAUER, MD (10/30/2020):
===================================
An ECG without History is Mystery. That’s the “theme” of today’s case. We emphasize often the potential utility of serial tracings — but without solid appreciation of the circumstances surrounding why and when the “previous tracing” was obtained — it is difficult to determine IF there has been meaningful change since this last ECG was recorded.
- Consider the 2 tracings shown in Figure-1. Imagine you had no history to go on. WHAT are your thoughts about these 2 ECGs?
Figure-1: Imagine you were asked to interpret the 2 ECGs in this figure without benefit of any history (See text).
MY Thoughts regarding Figure-1:
In the absence of a history — Isn’t it tempting to say that both tracings in Figure-1 show a number of “nonspecific” ST-T wave changes that probably are not acute?
- IF these ECGs appeared in a “pile” of tracings-to-be-read — Would one or both of them be worthy of further inquiry?
ECG #1 (in Figure-1):
The rhythm in ECG #1 is sinus at ~90/minute. There is indeed a series of subtle ST-T wave changes seen in multiple leads on this tracing. That said, in the absence of a history — I was initially tempted to interpret these changes in ECG #1 as probably not acute until I saw lead V2.
- Transition occurs unexpectedly early in ECG #1 (ie, the R wave abruptly becomes predominantly positive as soon as lead V2) — with a disproportionately tall T wave in lead V2 that is fatter-than-it-should-be at its base. There is also subtle-but-real J-point ST depression in lead V2.
- My IMPRESSION: As was true for me regarding my impression of the initial ECG in today’s case — I did not know what to make of ECG #1 until I learned the history. But even before learning the history in this case, in the context of the above-noted findings in lead V2 — the subtle-but-real ST-T wave changes in many of the other leads in ECG #1 could certainly indicate a very recent infero-postero-lateral MI.
- Learning the History supported the reason for my concern (ie, chest pain in this 50-something woman had begun ~12 hours prior to the time ECG #1 was recorded). Cardiac cath was ultimately done (albeit delayed) — and 100% occlusion of the Obtuse Marginal branch of the LCx (Left Circumflex) artery was found. The reason the T wave in lead V2 of ECG #1 is disproportionately tall and “fat”-at-its-base — is that this is a reperfusion T wave that developed as her posterior OMI evolved.
- NOTE: For full discussion on specifics of ECG #1 (including illustration of a positive Mirror-Test for the QRST complex in lead V2) — Please SEE My Comment at the bottom of the page of our October 2, 2020 post in Dr. Smith’s ECG Blog.
ECG #2 (in Figure-1):
The rhythm in ECG #2 is sinus at ~75/minute. There is nonspecific ST-T wave flattening in the limb leads. In the chest leads — R wave progression is normal. Criteria for LVH are not quite met.
- The remarkable finding in ECG #2 is the Wellens-like ST-T wave that is seen in leads V2-V4. By this I mean that the T wave in these leads remains upright — with rapid descent from the peak of the T wave into terminal T wave negativity. This Wellens-like ST-T wave picture begins (and is very subtle) in lead V2 — it is most prominent in lead V3 — and it is resolving in lead V4 (in which a persistent positive-then-negative biphasic T wave is still seen).
- The last 2 chest leads (ie, leads V5,V6) show ST segment coving (without elevation) and shallow inverted T waves (without any biphasic component).
- Learning the History was critical for clinical interpretation of ECG #2. This 50-something man gave a history of short-lived episodes of “squeezing” chest pain that had been intermittent over time — but which worsened the night before he presented to the ED. He had one more episode shortly before arriving at the ED — but he was completely pain-free at the time ECG #2 was recorded.
- My IMPRESSION: The association of the ECG findings seen in ECG #2 in this 50-something man with a history of cardiac chest pain, but who was completely pain-free at the time ECG #2 was recorded — is consistent with Wellens’ Syndrome!
- The ECG findings of Wellens’ Syndrome reflect anterior lead ST-T wave reperfusion changes from LAD occlusion (or near-occlusion), usually in the proximal portion of this artery. As in this case — the patient should be pain-free at the time the ECG showing Wellens-like ST-T wave changes is recorded — because there has been spontaneous reperfusion before infarction has occurred (or following no more than brief LAD occlusion that produces no more than minimal injury, thereby leaving R wave progression intact).
- NOTE: For full discussion by Dr. Smith on specifics of ECG #2 — Please SEE the November 15, 2013 post in Dr. Smith’s ECG Blog.
Additional LEARNING Points from Today’s Case:
The lesson from today’s case is clear. Deepening T wave inversion is part of the normal progression after reperfusion from a STEMI. Regardless of whether or not the deep T wave inversion in the 1st tracing shown from today’s case reflects a component of anginal chest pain — knowing the History (and seeing the sequence of recent ECGs in today’s case) told us that there was not re-occlusion of the “culprit” artery.
- Point #1: The patient in today’s case will not have a new “prior tracing” available for comparison in the event of a future ED visit until T wave inversion from her STEMI of 7 days earlier ceases to evolve.
- Point #2: Remember — An ECG without History is Mystery. Optimal clinical interpretation of the initial tracing in today’s case — as well as optimal clinical interpretation of ECG #1 and ECG #2 (in Figure-1) is simply not possible in the absence of a History.
- Point #3: Did YOU appreciate that the initial ECG shown in today’s case (above) + the 2 ECGs shown in my Figure-1 provide 3 examples of reperfusion T waves? (following OMIs involving inferior — posterior — and anterior lead locations, respectively).
- Point #4: The initial ECG shown in today’s case (above) — actually shows reperfusion T waves following not only inferior OMI (those very deep, inverted T waves in the inferior leads) — but also posterior OMI (the upright T wave in lead V2) + lateral OMI (the ST coving with shallow T inversion in leads V5, V6).









No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.