A 60-something male was sent from Dialysis for several days of SOB. He did not know his medical history well.
The patient was in no distress.
The paramedics recorded an ECG:
Here I magnify the limb leads and precordial leads:
The medics activated the cath lab. Do you agree?
I was in the ED, and whenever I hear that there has been a prehospital cath lab activation, I like to go take a look because there are many false positive activations, especially in patients without chest pain.
First: remember that a heart rate that fast is unusual in acute type 1 MI unless there is cardiogenic shock or impending shock. But the patient appears well.
Second: Look carefully at the limb leads: there are definite flutter waves.
You can also see them easily in lead V1 and V2: see the regular spikes at a rate close to 300?
Third: Whenever you see abnormal ST-T, look at the QRS. Here you see QS-waves, highly suggestive of old MI with persistent ST Elevation (LV aneurysm morphology -- LVA). Other reasons for QS-waves are LVH and cardiolmyopathy, and both can have baseline ST Elevation.
----Such baseline STE is often exaggerated by tachycardia.
----Flutter waves can also superimpose and exaggerate the ST Elevation.
My interpretation at the time I saw this: probably a false positive.
Plan? Let's get an ED ECG and look at old ECGs before confirming cath lab activation.
Here is the ED ECG:
Here is the Previous ECG recorded 2 months prior:
Here is an echo less than one year prior:
Mildly enlarged left ventricle with severely reduced systolic function.
The estimated ejection fraction is 16%.
Global hypokinesis with minor regional variations
Left ventricular hypertrophy concentric mild.
So it seems that the baseline ST Elevation may be due to LVH instead of LVA, but what matters is that there is baseline STE.
Here is another recent ECG:
Cath lab activation was cancelled.
The heart rate was controlled with beta blockers.
The patient was in no distress.
The paramedics recorded an ECG:
Here I magnify the limb leads and precordial leads:
 |
Now of course you see the convex ST elevation in V3 and V4, and the STE in V2 that is preceded by a spike.
Is this STEMI?
|
Here is the Computer Interpretation:
The medics activated the cath lab. Do you agree?
I was in the ED, and whenever I hear that there has been a prehospital cath lab activation, I like to go take a look because there are many false positive activations, especially in patients without chest pain.
First: remember that a heart rate that fast is unusual in acute type 1 MI unless there is cardiogenic shock or impending shock. But the patient appears well.
Second: Look carefully at the limb leads: there are definite flutter waves.
You can also see them easily in lead V1 and V2: see the regular spikes at a rate close to 300?
Third: Whenever you see abnormal ST-T, look at the QRS. Here you see QS-waves, highly suggestive of old MI with persistent ST Elevation (LV aneurysm morphology -- LVA). Other reasons for QS-waves are LVH and cardiolmyopathy, and both can have baseline ST Elevation.
----Such baseline STE is often exaggerated by tachycardia.
----Flutter waves can also superimpose and exaggerate the ST Elevation.
My interpretation at the time I saw this: probably a false positive.
Plan? Let's get an ED ECG and look at old ECGs before confirming cath lab activation.
Here is the ED ECG:
 |
| Same |
Here is the Previous ECG recorded 2 months prior:
 |
| This confirms previous QS-waves with baseline ST Elevation |
Here is an echo less than one year prior:
Mildly enlarged left ventricle with severely reduced systolic function.
The estimated ejection fraction is 16%.
Global hypokinesis with minor regional variations
Left ventricular hypertrophy concentric mild.
So it seems that the baseline ST Elevation may be due to LVH instead of LVA, but what matters is that there is baseline STE.
Here is another recent ECG:
 |
| It is identical to the presentation ECG! Atrial Flutter with rapid ventricular response, QS-waves, and exaggerated ST elevation |
Cath lab activation was cancelled.
The heart rate was controlled with beta blockers.
===================================
MY Comment by KEN GRAUER, MD (12/24/2019):
===================================
For Dr. Smith’s “Christmas Eve Special Gift” — I’ll limit my comments to brief review of my approach to this rhythm.
- For clarity in Figure-1 — I’ve lightened and simplified the initial tracing in this case ( = ECG #1, obtained by the paramedics on the scene).
QUESTION: How to go about determining the rhythm?
- HINT: I reviewed a nearly identical problem-solving approach in My Comment in the November 12, 2019 Post on Dr. Smith’s ECG Blog.
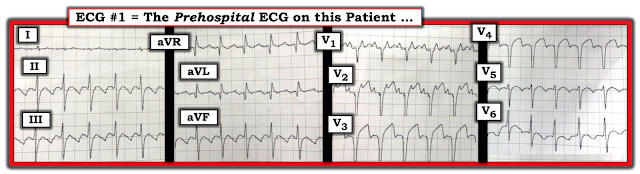 |
| Figure-1: The initial ECG shown in this case — obtained by the paramedics in the field. They were initially concerned about an acute STEMI ... (See text). |
ANSWER: As I describe in detail in my November 12, 2019 Post — As soon as you establish that this patient is hemodynamically stable — Proceed to Systematic Rhythm Analysis:
- The rhythm is regular at a rate of ~150/minute (ie, the R-R interval is ~2 large boxes on ECG grid paper — and 300/2 = 150/minute).
- The rhythm is supraventricular (ie, the QRS is narrow = not more than half a large box in duration).
- I do not clearly see sinus P waves. It almost looks like there is an upright P wave in lead II — but IF this upright deflection before each QRS in this lead was a P wave, then the PR interval would be fairly short. BOTTOM LINE: We are not certain there are sinus P waves in this tracing.
- EXTRA CREDIT: Look for sign of atrial activity in the other 11 leads. Look first at lead V1 — since next to lead II, lead V1 is often the best lead to search next for sign of atrial activity. Pull out your trusty pair of CALIPERS! Don’t YOU see 2 pointy spikes that regularly fall within the R-R interval of each beat in lead V1? Set your calipers to precisely the interval between 2 of these pointed peaks in lead V1 — and NOTE how you can precisely walk out these spikes at a rate of 300/minute throughout this lead V1. The only rhythm that does this (ie, give you regular atrial activity at ~300/minute) — is AFlutter — and you have just made a definitive diagnosis of the rhythm in Figure-1!
- SHORTCUT #1: Even before you got to the “Extra Credit” Step — Once you realized that the rhythm was a regular SVT at ~150/minute without clear sign of sinus P waves — You could have said to yourself, “Think AFlutter until proven otherwise” — and you would have then made a definitive diagnosis of this rhythm in less than 1 minute! (That's because AFlutter is by far the most commonly overlooked cardiac arrhythmia — and the BEST way to never again overlook AFlutter, is to always LOOK FOR IT whenever you have a regular SVT at ~150/minute without clear sign of sinus P waves!).
- SHORTCUT #2: Also before you got to the "Extra Credit" Step — Remember that when looking for AFlutter (because you have a regular SVT without clear sinus P waves at a rate close to ~150/minute) — it sometimes helps to STEP BACK a little from the tracing. Doing so should highlight the distinct "sawtooth" pattern of AFlutter that is strikingly prominent in the inferior leads of Figure-1. (Learning to recognize this "sawtooth" pattern facilitates recognizing many cases of AFlutter within seconds!).
HAPPY HOLIDAYS to ALL!
- IF in doubt about what to gift your special friend/colleague who loves ECG interpretation as much as you do — Gift them with a pair of CALIPERS! (Tell them Dr. Ken suggested this! — :)




The flutter waves are so obvious in leads II, III and aVF ("sloping up, sloping down, sloping up, sloping down" or "dome, dome, dome"), which are confirmed by lead V1. To some, the diagnosis of atrial flutter is so easy and fun, but to some, it is so difficult!!!
ReplyDeleteK. Wang.
THANKS so much K for your comment! I had MEANT to comment on the point you emphasize earlier — but in my “haste” to finish when I was writing a few hours ago, I forgot … Seeing your comment just now “jogged my memory” — so I just now added “Shortcut #2” to highlight the important point you raise. THANK YOU! I also agree entirely with you that once providers become “used to” HOW to recognize AFlutter — it often becomes far easier to identify this rhythm within seconds. And then, it only take 2-3 seconds more to verify 2:1 AV conduction (and PROVE your diagnosis) with the use of your calipers — :)
DeleteNo, but that would not help very much. First, 25% of STEMI have a first troponin below the 99th %-ile, and 50% have a first troponin below the often published value as diagnostic for MI (52-64 ng/mL, with almost any assay, I or T). So you cannot depend on that.
ReplyDeleteHas that atrial flutter reverted with beta blocker??
ReplyDeleteThe rate was controlled (last sentence by Dr. Smith in his comment above) — but NO mention of conversion to sinus rhythm in the ED with a beta-blocker. I believe follow-up during the hospital course is often lost for ED providers ... In general, a beta-blocker is a reasonable medication for rate control — but not for conversion to sinus rhythm when the rhythm is atrial flutter ...
Delete