This was written by Magnus Nossen from Norway
The patient is female in her 80s with a medical hx of previous MI with PCI and stent placement. She also has a hx of paroxysmal atrial fibrillation and is on oral anticoagulant treatment. She had a single chamber ICD/Pacemaker implanted several years prior due to ventricular tachycardia. The last echocardiography 12 months ago showed HFmrEF.
She presented to the emergency department after a couple of days of chest discomfort.
The ECG below was recorded.
What is your assessment? How would you manage this patient?
If the patient is hemodynamically stable, iv amiodarone could be considered in such a clinical situation. However, this patient is having chest discomfort, and by definition then she should be considered not to be stable.
Is this:
1. Primary VT, and the VT with tachycardia is causing ischemia with chest discomfort (supply-demand mismatch/type 2 MI)? Or
2. Ischemia from ACS causing the chest discomfort, with VT another consequence (or coincidence)?
In either case, prompt cardioversion is indicated.
Cardioversion will address the rhythm problem immediately, also if the chest discomfort subsides when SR is restored, ischemia from ACS becomes much less likely.
The ECG in sinus rhythm will also be more easy to assess with regards to ischemia
The VT was not appreciated and patient was admitted with telemetry and IV amiodarone. During the night the rhythm changed. How do you interpret the below ECG?
The above ECG shows a ventricular paced rhythm with a heart rate of 60. Pacing spikes are most easily appreciated in the inferior and early precordial leads. There is retrograde conduction through the AV node with retrograde P waves best seen superimposed on the last part of the QRS. (Most readily seen in V1, red arrows)
After the VT had terminated, the patient became hypotensive, with cool and clammy skin. A bed side echocardiography revealed a severely depressed LVEF of about 20-25%.
The pacing rate was increased without clinical improvement and the patient was transferred to the ICU for closer monitoring/treatment. When looking at the above ECG you will find that the QRS following ventricular pacing is very long. The QRS duration measured in lead II (shown below) is about 6.5 small squares in width (260ms). This is very prolonged. Such a QRS duration inevitably is associated with profound ventricular dyssynchrony. Seeing as the patient has a single chamber ICD/pacemaker, pacing the ventricle will also lead to AV dyssynchrony that will compromise ventricular filling, further impairing hemodynamics.
It was apparent that the ventricular pacing was detrimental to the patient’s hemodynamics. The ICD/pacer back up rate was lowered to 40/min (VVI 40) in an attempt to promote intrinsic activity and intrinsic AV conduction.
The above ECG was recorded after the lower rate limit (LRL) of the ICD/pacer was set @40bpm. The ECG shows what is likely an atrial ectopic rhythm with a left anterior hemiblock. There are QS-waves in V1-V4 with a fragmentation/notch in the last part of the QRS. There is some STE.
These are all findings that can be expected with left ventricular aneurysm.
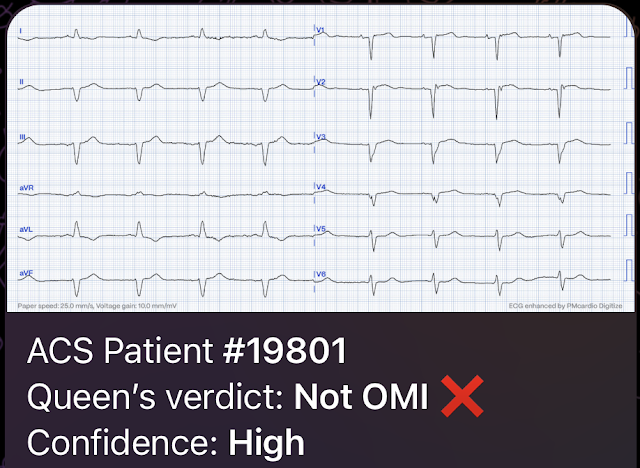
This ECG does not show any sign of OMI.
The assessment of the ST segments and T waves for ischemic changes can be done with much more confidence once normal rhythm and impulse propagation is restored. The Queen of Hearts also recognizes that this pattern of STE is not indicative of active ischemia and her interpretation is NOT OMI with high confidence.
Summary: This patient had a CTO (chronic total occlusion) of the LAD since many years prior with a known LVA on echocardiography. Slow VT below the detection rate of the ICD lead to worsening heart failure and low stroke volume. Cardiac output (CO) was being maintained by the tachycardia. Post conversion of VT the patient had low output cardiac failure and became unstable and hypoperfused. Ventricular pacing was detrimental with regards to hemodynamics. Lowering the back up rate (LRL) of the ICD/pacer allowed for an intrinsic rhythm with physiologic AV conduction and normal AV synchrony with resultant increase in stroke volume and cardiac outpt. After atrial rhythm/SR was restored the patient slowly improved. Medical treatment for heart failure was optimized and after a few days the patient was discharged with referral to VT ablation procedure.
Learning points
*A patient with tachydysrhythmia and chest discomfort needs immediate rhythm or rate control.
*Sometimes a slower rate with intrinsic conduction gives better CO than higher rate pacing.
*Temporarily decreasing the LRL of the ICD/Pacemaker can promote intrinsic depolarization which is beneficial when assessing ST segments and T waves for ischemia.
MY Comment, by KEN GRAUER, MD (1/10/2024):
- The patient is an older woman with known coronary disease and an ICD-Pacemaker implanted because of a history of VT (Ventricular Tachycardia). The patient also has a history of AFib and HFmrEF ( = Heart Failure with Minimally-Reduced Ejection Fraction).
- This patient presented to the ED “after a couple of days of chest discomfort”.
For clarity in Figure-1 — I have reproduced and labeled this patient’s initial ECG.
QUESTION:
- For HOW LONG has this patient been in VT?
-USE.png) |
| Figure-1: I have labeled the initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- Given the above scenario — there is much to comment on ...
- While fully acknowledging that "Sometimes ya gotta be there!" — in order to optimally assess the patient — the clinical definition of hemodynamic stability is for the patient to be without significant symptoms such as chest pain, shortness of breath, hypotension and/or mental status changes — as a direct result of the fast heart rate.
- As per Dr. Nossen — the fact that today's patient was having chest discomfort in association with the rhythm in Figure-1 — meant that by definition, this patient was hemodynamically "unstable" — with clear indication for immediate cardioversion instead of being treated with IV amiodarone over a period of hours.
- KEY Point: Additional historical features in today's case that strongly favor electrical cardioversion sooner rather than later include: i) Older age of the patient (ie, this 80-year old woman being less likely to tolerate any sustained tachycardia for an extended period of time); ii) A known medical history of coronary disease, heart failure and documented sustained VT in the past; — and, iii) Statistical likelihood that even before we look at this patient's ECG — there is a greater than 90% chance that she is in sustained VT.
- The ECG in Figure-1 is a regular WCT ( = Wide-Complex Tachycardia) at ~130/minute, without clear sign of sinus P waves. Pre-Test Likelihood that a regular WCT without P waves will turn out to be VT is ~80% in the literature. This figure goes up to ~90% Pre-Test Likelihood — IF the patient is "older" (ie, an adult of a "certain" age) — and if the patient has underlying heart disease. As a result — Statistical Likelihood that the regular WCT without P waves in Figure-1 will turn out to be VT is at least 90% even before we look at the actual ECG!
- Because of this 1st bullet — We need to always assume VT for such rhythms until we prove otherwise, and treat accordingly. This does not mean that all patients need to be immediately shocked — but it does mean that since 90+% of such rhythms will turn out to be VT, that we need to assume VT until proven otherwise. This was not done by the treating clinicians in today's case.
- Now that we are looking closer at ECG #1 — reasons why statistical likelihood of VT goes up to over 95-98% in today's case are: i) The QRS complex is exceedingly wide (Using the vertical BLUE line as the starting point of the QRS — and the vertical YELLOW line as the end point of the QRS — QRS duration is >0.16 second); ii) There is almost extreme axis deviation (ie, the QRS is all negative in lead III — albeit not all negative in lead aVF); iii) There is delay in initial activation (ie, Note especially how long it takes for the QS complex in lead V4 to reach its lowest point); and, iv) QRS morphology does not resemble any known form of conduction defect.
- It is this last criterion (ie, not resembling any known form of conduction defect) — that is the most suggestive of VT to me in today's case. Although there is superficial resemblance of QRS morphology to LBBB conduction (because of the upright QRS in leads I,aVL,V6 — and the predominantly negative complexes in leads V1-thru-V4) — closer scrutiny suggests extremely atypical morphology for LBBB conduction in multiple leads. This highly atypical morphology includes: i) Exceeding wide initial Q waves in leads I,II (within the dotted RED ovals in these leads) — and in aVL,V5,V6 (wide Q waves like this are virtually never seen with supraventricular conduction in these leads); — and, ii) An extremely wide initial R wave in lead V1 (within the dotted RED oval — with this morphology also virtually never seen with LBBB conduction that never normally manifests more than a small, slender initial r wave in lead V1).
- To Emphasize: Statistical odds of over 90-95% is not the same as 100% likelihood. There is almost always the possibility of exceptions (ie, prior infarction or cardiomyopathy that might result in a very abnormal baseline tracing). But over 95% likelihood in today's case supports the need to assume VT until proven otherwise.
- Atrial activity with AFlutter is extremely regular — and typically manifests a "sawtooth" pattern, that most often is seen in one or more of the following leads = leads II,III,aVF; aVR; and/or lead V1. However, there is no "sawtooth" pattern to the rhythm in Figure-1. The treating clinician mistook the 2 negative deflections within each R-R interval of lead I as "flutter activity" — but it would be highly unusual to only see flutter waves in lead I, but not in any of the 5 leads I cited above.
- I've drawn vertical RED lines under the negative deflections for a series of beats in lead I. It should be immediately obvious that the interval between each of these vertical RED lines is not equal (whereas with AFlutter — there typically is precise equality in the intervals between one flutter wave and the next).
- Instead (as per Dr. Nossen) — there is retrograde atrial conduction every-other-beat, in the form of a negative P wave that occurs at a fixed RP' distance after every-other-QRS complex (YELLOW arrows seen in each of the inferior leads). This intermittent 2:1 retrograde atrial block is consistent with VT — but rules out any possibility of AFlutter.
- PEARL: I find using calipers is the most time-efficient way of diagnosing AFlutter with relative certainty from an initial ECG. Starting from the premise that AFlutter should always be considered until proven otherwise in any regular supraventricular rhythm at a rate close to 150/minute (ie, 130-170/minute range) when sinus P waves are not clearly seen — I set my calipers to precisely half the R-R interval. IF the rhythm is AFlutter — then I will almost always be able to precisely "walk out" 2:1 atrial activity in one or more leads on the tracing. Using calipers — it literally takes me no more than seconds to verify 2:1 AV conduction.
- Lewis Leads: Use of another lead system is an easy-to-do but often forgotten application — that can be highly effective for revealing underlying atrial activity that was not evident on the standard ECG tracing (Please see my last Figure in the November 12, 2019 post of Dr. Smith's Blog for a reminder on how to apply Lewis Leads).
- Remember that this patient presented to the ED “after a couple of days of chest discomfort”. The heart rate during the WCT rhythm was not overly fast (ie, ~130/minute). And, presumably from the history we are provided with — no ECG was done during the "couple of days with chest discomfort" until the patient finally presented to the ED, and ECG #1 was recorded.
- As I discussed in My Comment at the bottom of the page in the April 2, 2022 post in Dr. Smith's ECG Blog — I am aware of many cases of sustained VT in which the patient remained awake and alert for hours. I'm also aware a number of cases (including one at my former hospital) — where the patient was awake and alert in sustained VT for several days! Therefore — Just because a patient remains awake and alert with an adequate blood pressure for an extended period of time does not rule out the possibility sustained VT. If the ventricular rate is not excessively fast — and the patient has reasonable LV function — then it is possible possible to remain in sustained VT for hours, and even days.
- The literature supports the premise that it is possible to remain in sustained VT for days at a time (Symanski & Marriott — Heart-Lung 24:121,123, 1995). In this case report — the 69-year old woman (who incidently had a history of both coronary disease and cardiomyopathy) — remained in sustained VT for 5 days without hemodynamic deterioration. During this time, she was treated in the hospital with multiple antiarrhythmic medications including Adenosine, Verapamil and Digoxin. On her 5th hospital day — she was given Amiodarone, which successfully converted the rhythm. Luckily — she "survived" the above treatment course (as each of the first 3 drugs that were given could have been fatal, given their tendency to precipitate VT deterioration in the setting of severe underlying coronary disease).
- To Emphasize: This case study by Symanski and Marriott is from 1995. Many advances in treatment have occurred in the 28 years since this article was published. That said — misdiagnosis of WCT rhythms for the same reasons cited by the authors remains all-too-common — so the lessons put forth in this 1995 article remain relevant. I suspect the patient in today's case may have been in sustained VT since the onset of her chest discomfort, that began "a couple of days earlier" — but this possibility was discounted because her physicians did not believe that anyone could remain alert and hemodynamically stable in sustained VT for "a couple of days".






No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.